- What Is NLP, and How Does It Work in Telemedicine?
- Key Applications of NLP in Telemedicine
- Benefits of implementing NLP in telemedicine platforms
- How to Implement NLP in Your Telemedicine Platform
- Challenges and Considerations for NLP in Healthcare
- Real-world examples of NLP in telemedicine
- Build Smart, NLP-Enabled AI Telemedicine Solutions with Space-O AI
- Frequently Asked Questions on NLP in Telemedicine
- 1. What is NLP in telemedicine, and how does it improve patient care?
- 2. How accurate is NLP for medical documentation?
- 3. Is NLP in telemedicine HIPAA compliant?
- 4. What is the cost of implementing NLP in a telehealth platform?
- 5. How long does it take to implement NLP in telemedicine?
- 6. Can NLP handle multiple languages in telemedicine applications?
- 7. What is the difference between NLP and generative AI in healthcare?
NLP in Telemedicine: How Natural Language Processing Transforms Virtual Healthcare

Telemedicine has transformed access to healthcare, but virtual care still generates massive volumes of unstructured data through clinical notes, chat conversations, voice calls, and patient messages. Extracting actionable insights from this data at scale remains one of the biggest challenges healthcare providers face today.
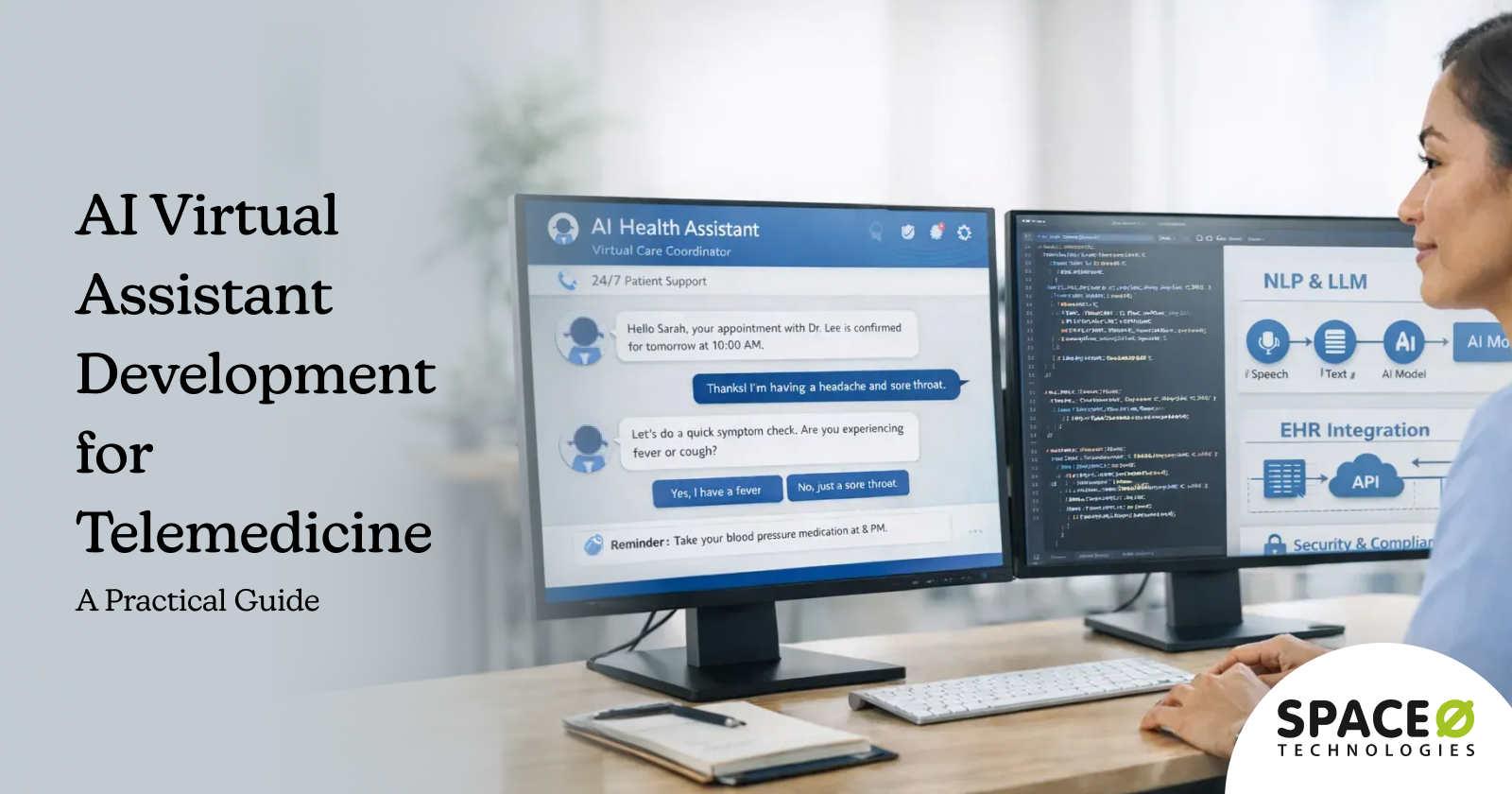
This is where Natural Language Processing in telemedicine plays a critical role. NLP enables telemedicine platforms to understand, interpret, and analyze human language across text and voice interactions. From automating clinical documentation and triaging patient symptoms to powering conversational AI and analyzing patient sentiment, NLP helps healthcare teams deliver faster, more accurate, and more personalized virtual care.
The growing importance of NLP in healthcare is reflected in market growth. According to Nova One Advisor, the NLP in the healthcare and life sciences market is projected to reach approximately USD 118.41 billion by 2034. This highlights how rapidly healthcare organizations are investing in language-driven AI technologies to improve care delivery and operational efficiency.
In this blog, we explore how NLP is used in telemedicine, key use cases, benefits, and implementation considerations. We have shared expert tips and insights as a leading healthcare AI development company to help you implement NL-powered telemedicine solutions in your practice. Let’s get started.
What Is NLP, and How Does It Work in Telemedicine?
Natural Language Processing, or NLP, is a branch of artificial intelligence that enables computers to understand, interpret, and generate human language. In healthcare, NLP is used to analyze both written and spoken medical information such as clinical notes, patient messages, transcripts from virtual visits, and voice interactions.
In telemedicine, NLP works by converting unstructured language data into structured, actionable insights. Patient inputs from chat, email, voice calls, or intake forms are first captured and cleaned. NLP models then process this data using techniques like entity recognition, intent detection, sentiment analysis, and context understanding.
This allows the system to identify symptoms, medications, diagnoses, care instructions, and patient intent accurately.
For example, during a virtual consultation, NLP can transcribe and summarize the conversation, extract key clinical details, and automatically update electronic health records. In patient-facing applications, NLP powers chatbots and virtual assistants that understand natural language questions, guide patients through symptom assessment, and route requests to the appropriate care team. NLP is also used to analyze patient feedback and communication patterns to detect risk signals, follow-up needs, or declining engagement.
Clinical NLP vs generic NLP: Key differences
- Domain-specific vocabulary: Medical terminology includes thousands of specialized terms, drug names, and procedure codes
- Abbreviation complexity: Healthcare uses extensive abbreviations that vary by specialty and institution
- Negation handling: Clinical notes frequently describe what patients do not have, requiring systems to detect and process negations correctly
- Uncertainty detection: Clinicians express varying degrees of certainty that NLP must capture, such as “possible pneumonia” versus “confirmed pneumonia.”
- Temporal reasoning: Understanding when symptoms started, when medications were taken, and the sequence of clinical events
The goal is to transform unstructured clinical language into structured, actionable data. When a patient describes symptoms during a video visit, NLP can extract relevant clinical concepts, suggest appropriate documentation, and even flag potential concerns for the clinician. This brings us to the specific applications where NLP delivers the most value in telemedicine settings.
Key Applications of NLP in Telemedicine
Across the different use cases of AI in telemedicine, NLP serves multiple functions within telemedicine platforms. Each application addresses specific workflow challenges that healthcare organizations face when delivering virtual care. Here are the primary use cases where NLP creates a measurable impact.
1. Clinical documentation and note processing
Documentation consumes substantial clinician time during and after patient encounters. NLP-powered documentation tools address this burden through several mechanisms.
- Real-time transcription converts spoken conversations during video consultations into text. The system captures the dialogue between clinician and patient, creating a foundation for clinical notes without manual typing.
- Clinical summarization goes beyond transcription. NLP analyzes the full conversation and generates structured summaries organized by clinical relevance. The system can identify chief complaints, history of present illness, review of systems, and assessment details from natural conversation.
- SOAP note generation structures extracted information into the standard Subjective, Objective, Assessment, and Plan format. Clinicians review and approve the generated notes rather than creating them from scratch.
- Structured data extraction pulls discrete data elements from narrative text. When a patient mentions medications, allergies, or symptoms, NLP identifies and codes these elements for integration with electronic health records.
2. Medical coding automation
Medical coding translates clinical documentation into standardized codes for billing and reporting. This process is time-consuming and error-prone when done manually.
- ICD-10 code suggestion analyzes clinical notes and recommends appropriate diagnosis codes based on documented conditions. The system identifies relevant terms and maps them to the corresponding codes.
- CPT code recommendation works similarly for procedure codes. NLP identifies documented services and suggests appropriate billing codes for the encounter.
- Coding accuracy improvement reduces claim denials caused by coding errors or mismatches between documentation and submitted codes. The system flags potential issues before claims submission.
- Revenue cycle optimization results from faster, more accurate coding. Claims process more quickly, denial rates decrease, and reimbursement improves.
3. Patient communication analysis
Telemedicine platforms generate substantial patient communication through portals, chat interfaces, and messaging systems. NLP helps organizations manage and respond to this volume effectively.
- Symptom extraction identifies clinical information from patient messages. When patients describe how they feel, NLP extracts relevant symptoms and clinical concepts for clinician review.
- Triage and prioritization classify incoming messages by urgency. The system can identify messages requiring immediate attention versus routine follow-ups, helping staff manage their queues efficiently.
- Sentiment analysis evaluates patient satisfaction and emotional state from written communications. This helps organizations identify frustrated patients, track satisfaction trends, and intervene when needed.
- Automated response generation drafts appropriate replies to common patient inquiries. Staff review and send responses rather than composing them from scratch, reducing response time.
4. Clinical decision support
NLP enhances clinical decision-making by extracting and organizing relevant information from various sources.
- Evidence-based recommendations surface relevant clinical guidelines based on documented patient conditions. The system connects patient data with appropriate care protocols.
- Drug interaction detection identifies potential medication conflicts by analyzing prescribed and documented medications. NLP extracts drug names from notes and checks for interactions.
- Adverse event identification monitors patient communications and documentation for signals of potential complications or side effects requiring attention.
- Clinical trial matching compares patient characteristics extracted from documentation against trial eligibility criteria to identify potential research opportunities.
These applications work together to create more efficient telemedicine workflows. Organizations typically start with one or two high-priority use cases and expand over time. Now, let us examine the specific benefits that drive NLP adoption in telemedicine settings.
Turn Telemedicine Conversations Into Actionable Insights with NLP
Our NLP experts help healthcare organizations extract clinical and operational intelligence from patient interactions.
Benefits of implementing NLP in telemedicine platforms
Healthcare organizations invest in NLP for telemedicine to achieve specific operational and clinical improvements. Understanding these benefits helps leaders evaluate whether NLP aligns with their strategic priorities.
1. Reduced documentation burden
Clinical documentation represents one of the largest time investments for healthcare providers. NLP-powered tools significantly reduce this burden.
Clinicians can focus more on patient interaction during video consultations rather than typing notes simultaneously. The system captures the conversation and generates documentation for review. This shift improves both clinician satisfaction and patient experience during virtual visits.
Post-visit documentation time decreases when clinicians review and approve AI-generated notes rather than creating them manually. This efficiency gain translates to more patients seen or a better work-life balance for providers.
2. Improved coding accuracy and revenue
Medical coding errors lead to claim denials, payment delays, and revenue leakage. NLP reduces these issues through consistent, systematic code suggestion.
The technology applies the same logic across all encounters, reducing variation that occurs with different human coders. It identifies documentation gaps that might result in undercoding and flags potential compliance issues before claim submission.
Organizations implementing NLP for coding support typically see measurable reductions in denial rates and improvements in time to reimbursement. The financial impact often provides a clear return on investment for NLP initiatives.
3. Enhanced patient engagement
NLP enables more responsive and personalized patient communication at scale. Telemedicine platforms handle substantial message volume that would otherwise require proportional staff increases.
Automated triage ensures urgent messages receive immediate attention while routine inquiries are handled efficiently. Patients experience faster response times, improving their perception of care quality.
Sentiment analysis helps organizations identify patients who may be dissatisfied or struggling. Proactive outreach to these patients can improve retention and outcomes.
4. Better clinical insights
Unstructured clinical data contains valuable information that remains inaccessible without NLP. Extracting and analyzing this data enables population health insights and quality improvement.
Organizations can identify patterns across patient populations, track outcomes for specific conditions, and measure adherence to care protocols. These insights inform clinical program development and resource allocation.
Real-time analysis during consultations surfaces relevant patient history and clinical context. Clinicians make more informed decisions when they have complete, organized information available.
5. Operational scalability
NLP allows telemedicine operations to scale without proportional increases in administrative staff. As patient volume grows, NLP handles increased documentation, coding, and communication workload.
This scalability is particularly valuable for organizations experiencing rapid telemedicine growth. The technology provides a path to manage volume increases while maintaining quality and response times.
With these benefits in mind, let us explore how organizations actually implement NLP in their telemedicine platforms.
How to Implement NLP in Your Telemedicine Platform
Implementing NLP in telemedicine requires careful planning across technical, operational, and compliance dimensions. This section provides a framework for approaching NLP implementation systematically.
1. Assessing your NLP readiness
Before selecting NLP solutions, organizations should evaluate their current state across several dimensions. An AI readiness assessment can help understand determine how prepared an organization is to implement NLP telemedicine solutions.
- Data availability and quality determine what NLP can accomplish. Assess the volume and format of clinical documentation, patient messages, and transcripts available for processing. Consider whether historical data exists for model training or if you will start with pre-trained models.
- Integration requirements shape technical decisions. Document your current EHR/EMR system, telemedicine platform, and other clinical applications. Identify where NLP outputs need to flow and what integration methods each system supports.
- Compliance and security posture establish constraints. Review your current HIPAA compliance program, data handling policies, and security infrastructure. Determine whether cloud-based or on-premise deployment aligns with your requirements.
- Organizational readiness affects adoption. Evaluate clinician and staff attitudes toward AI-assisted tools. Identify champions who can support rollout and resistors whose concerns need addressing.
2. Choosing the right NLP approach
Several technical approaches exist for implementing NLP in healthcare. The right choice depends on your specific requirements and constraints.
- Pre-trained medical NLP models offer faster time to value. Models like BioBERT, ClinicalBERT, and PubMedBERT are trained on medical literature and clinical text. They understand healthcare terminology out of the box and can be fine-tuned for specific use cases.
- Large language models (LLMs) like GPT-4 and Claude provide powerful general language capabilities. These models require careful prompt engineering and may need fine-tuning for clinical accuracy. They excel at summarization and generation tasks but require validation for medical applications.
- Custom model development provides maximum control and optimization for specific use cases. This approach requires more data, time, and expertise but can achieve higher accuracy for narrow, well-defined tasks.
- Build versus buy decisions require honest assessment. Commercial NLP solutions offer faster deployment and proven capabilities. Custom development provides differentiation and control but requires sustained investment. Many organizations use commercial platforms as a foundation with custom components for specific needs.
3. Integration with clinical workflows
Technical implementation must align with how clinicians and staff actually work. Poor workflow integration leads to low adoption regardless of technical capability.
- EHR/EMR integration is typically essential. NLP outputs should flow into clinical documentation systems without requiring separate logins or copy-paste workflows. Evaluate integration options, including APIs, HL7/FHIR interfaces, and vendor-specific connectors.
- Real-time versus batch processing depends on the use case. Real-time transcription and decision support require immediate processing. Coding suggestions and analytics can run as batch processes on completed documentation.
- Human-in-the-loop validation maintains quality and builds trust. Design workflows where clinicians review and approve NLP outputs rather than accepting them automatically. This catches errors, provides training feedback, and keeps clinicians appropriately engaged.
- Feedback mechanisms enable continuous improvement. Create easy ways for users to flag errors or provide corrections. Use this feedback to refine models and improve accuracy over time.
Professional AI integration services help organizations connect NLP capabilities with existing clinical systems effortlessly. Proper integration is often the difference between successful adoption and expensive shelfware.
Need Help Planning Your NLP Implementation?
Work with Space-O AI to design and implement NLP solutions that automate documentation, enhance virtual consultations, and improve clinical efficiency.
Challenges and Considerations for NLP in Healthcare
NLP implementation in telemedicine involves real challenges that organizations must anticipate and address. Transparent understanding of these issues leads to better planning and more successful deployments.
1. Medical language complexity
Healthcare language presents unique difficulties for NLP systems that general-purpose models cannot handle out of the box. Clinical text differs substantially from everyday language in structure, vocabulary, and conventions. Abbreviations like “PT” can mean physical therapy, patient, prothrombin time, or posterior tibial depending on context.
Clinicians frequently document negations (“no evidence of malignancy”) and uncertainty (“possible early pneumonia”) that require specialized handling. Additionally, documentation styles vary widely between providers, with some writing detailed narratives while others use brief phrases or shorthand.
How to overcome this challenge
- Deploy clinical NLP models pre-trained on medical corpora such as BioBERT, ClinicalBERT, or PubMedBERT that understand healthcare terminology
- Implement specialized negation detection algorithms (like NegEx or its successors) to accurately process clinical language
- Build institution-specific abbreviation dictionaries and train models on your organization’s documentation patterns
- Use LLM development services to fine-tune language models on your clinical data for higher accuracy
- Establish regular model updates as new medications, procedures, and terminology enter clinical practice
2. Data privacy and HIPAA compliance
Healthcare NLP processes protected health information (PHI), triggering strict regulatory requirements under HIPAA, HITECH, and other privacy frameworks. Organizations must navigate complex questions about using patient data for model training, storing processed information, and transmitting PHI to cloud-based NLP services.
The consequences of compliance failures include significant financial penalties, reputational damage, and potential harm to patients whose information is exposed.
How to overcome this challenge
- Conduct thorough privacy impact assessments before deploying any NLP solution that processes PHI
- Establish robust business associate agreements (BAAs) with all vendors whose systems handle patient data
- Implement proper de-identification pipelines validated against HIPAA Safe Harbor or Expert Determination standards
- Deploy on-premise NLP solutions when cloud transmission of PHI creates unacceptable risk
- Build comprehensive audit trails and access controls into every NLP workflow
- Partner with healthcare AI consulting experts who understand both the technology and regulatory requirements to ensure compliance from the start
3. Accuracy and clinical validation
NLP errors in healthcare carry higher stakes than in other domains. A misclassified symptom, missed medication interaction, or incorrect coding suggestion can affect patient care and reimbursement.
Organizations must establish rigorous validation frameworks that account for the specific risks of each use case, recognizing that documentation assistance may tolerate different error rates than clinical decision support. The challenge compounds because NLP accuracy can degrade over time as clinical practices evolve and new treatments emerge.
How to overcome this challenge
- Define clear accuracy thresholds for each use case based on clinical risk and intended use
- Validate models on representative datasets that reflect your patient population demographics and clinical scenarios
- Implement human-in-the-loop workflows where clinicians review and approve NLP outputs before they affect care or billing
- Establish continuous monitoring systems that detect performance degradation and trigger retraining
- Leverage MLOps consulting to build robust pipelines for model versioning, testing, and deployment that maintain accuracy over time
- Create feedback mechanisms allowing clinicians to flag errors and contribute to ongoing model improvement
4. Multilingual and dialect considerations
Telemedicine serves increasingly diverse patient populations who communicate in different languages, dialects, and accents. Most clinical NLP models are trained primarily on English text, leaving significant gaps for organizations serving multilingual communities.
Beyond translation, cultural differences affect how patients describe symptoms and conditions. Speech recognition components may struggle with regional accents, non-native speakers, or patients with speech impairments, creating barriers to accurate clinical documentation.
How to overcome this challenge
- Evaluate NLP vendors specifically on their language coverage for your patient population demographics
- Deploy separate specialized models for different languages rather than relying on translation layers
- Train speech recognition systems on diverse accent and dialect samples representative of your patients
- Implement quality assurance processes that specifically test accuracy across language and demographic groups
- Consider AI healthcare solutions designed with multilingual capabilities built in from the ground up
- Provide fallback options, such as human interpreters, when NLP confidence scores indicate potential accuracy issues
5. Integration and technical complexity
Connecting NLP capabilities with existing clinical systems presents technical challenges that extend beyond the NLP models themselves. Legacy EHR systems may lack modern APIs, requiring custom integration development.
Real-time use cases like transcription and decision support demand low-latency responses that constrain architecture choices. As telemedicine volume grows, NLP infrastructure must scale to handle peak loads during busy clinical hours without degradation or downtime.
How to overcome this challenge
- Conduct detailed integration assessments covering your EHR, telemedicine platform, and other clinical applications before vendor selection
- Prioritize NLP solutions with native HL7 FHIR support for standardized healthcare data exchange
- Design hybrid architectures that process time-sensitive requests locally while offloading batch analytics to cloud infrastructure
- Build scalable infrastructure with auto-scaling capabilities to handle volume fluctuations
- Work with AI integration specialists who understand both healthcare systems and modern AI deployment patterns
- Plan for phased rollouts that validate integration stability before expanding to full production volume
Understanding these challenges helps organizations plan realistic implementations. Many challenges are manageable with proper planning, but underestimating them leads to failed projects. With this realistic view established, let us look at how organizations are successfully applying NLP in telemedicine today.
Real-world examples of NLP in telemedicine
NLP applications in telemedicine have moved from experimental pilots to production deployments across healthcare organizations. These examples illustrate how different organizations apply NLP to address specific operational challenges.
1. Ambient clinical intelligence for virtual visits
Health systems are deploying ambient documentation systems that listen to telemedicine consultations and generate clinical notes automatically. During a video visit, the system captures the conversation between clinician and patient, identifies clinically relevant content, and structures it into SOAP-formatted documentation.
Clinicians conduct visits naturally, focusing on patients rather than keyboards, then review and approve generated notes after the encounter.
Key outcomes
- Clinicians maintain eye contact with patients throughout virtual visits instead of typing
- Documentation workflow shifts from creation to review, reducing cognitive load
- Post-visit charting time decreases significantly as providers approve rather than write notes
- Patient satisfaction improves when providers are fully present in conversations
- Note quality becomes more consistent across providers and encounter types
Organizations looking to implement ambient documentation benefit from generative AI development services to build systems that accurately capture and structure clinical conversations.
2. Patient message triage and response
Large telemedicine operations receive substantial volumes of patient messages through portals and apps. NLP analyzes incoming messages, classifies them by urgency and topic, and routes them to appropriate queues. Messages describing concerning symptoms receive priority routing to clinical staff, while routine inquiries about appointments or refills go to administrative teams.
Key outcomes
- Urgent messages surface immediately instead of waiting in chronological queues
- Response times improve as staff handle categorized message batches efficiently
- Draft response generation reduces time spent composing routine replies
- Sentiment analysis flags frustrated patients for proactive intervention
- Staff workload balances more evenly across clinical and administrative teams
3. Medical coding support
Healthcare organizations use NLP to assist with medical coding for telemedicine encounters. The system analyzes completed documentation and suggests appropriate ICD-10 diagnosis codes and CPT procedure codes. Coders validate suggestions rather than reading through entire notes to identify codeable elements, fundamentally changing their workflow from identification to verification.
Key outcomes
- Coding turnaround time decreases as coders review rather than search
- Consistency improves with standardized code suggestions across encounters
- Documentation gaps surface before claims submission, reducing denials
- Revenue capture increases when NLP identifies missed coding opportunities
- Telemedicine and in-person encounters receive consistent coding treatment
4. Clinical trial eligibility screening
Academic medical centers and research organizations use NLP to identify potential clinical trial participants from telemedicine patient populations. The system analyzes patient documentation against trial eligibility criteria and flags potential matches for research coordinators to review. This automated screening expands the pool of patients considered for trials beyond those whose providers happen to remember relevant studies.
Key outcomes
- Trial enrollment accelerates with systematic patient identification
- More eligible patients receive opportunities to participate in research
- Coordinator’s time shifts from manual chart review to candidate outreach
- Rare disease trials find qualified participants across larger patient bases
- Protocol amendments trigger automatic re-screening of patient populations
5. Symptom checker and pre-visit intake
Telemedicine platforms deploy NLP-powered symptom checkers that gather clinical information before virtual visits. Patients describe their symptoms in natural language, and the system extracts relevant clinical concepts to populate pre-visit summaries. Clinicians review these summaries before joining video consultations, entering visits informed about patient concerns and relevant history.
Key outcomes
- Clinicians start visits with structured symptom information already captured
- Visit time focuses on examination and discussion rather than history gathering
- Triage accuracy improves with systematic symptom assessment
- Urgent presentations route to expedited appointments or emergency referrals
- Patient experience improves with shorter, more focused consultations
6. Multilingual patient communication
Healthcare organizations serving diverse populations use NLP for multilingual communication support. The technology translates patient messages for clinical staff and generates responses in patients’ preferred languages. Beyond simple translation, medical NLP systems handle clinical terminology appropriately across languages and normalize cultural variations in symptom description.
Key outcomes
- Language barriers no longer prevent patients from accessing telemedicine services
- Clinical staff respond to messages without waiting for interpreter availability
- Consistent care quality across patient language preferences
- Reduced interpreter costs for routine asynchronous communication
- Broader patient populations served without proportional staffing increases
These implementations demonstrate that NLP in telemedicine is practical and valuable when implemented thoughtfully. Organizations achieve meaningful results by focusing on specific, well-defined use cases and expanding from proven successes.
Build NLP-Powered Telemedicine Workflows
Work with Space-O AI to design and implement NLP solutions that automate documentation, enhance virtual consultations, and improve clinical efficiency.
Build Smart, NLP-Enabled AI Telemedicine Solutions with Space-O AI
NLP in telemedicine delivers measurable improvements across clinical documentation, medical coding, patient communication, and decision support. Organizations that implement NLP strategically reduce administrative burden, improve coding accuracy, and enable clinicians to focus on what matters most: patient care.
Space-O AI brings 15+ years of AI development expertise and over 500 successfully developed and delivered AI projects. Our team understands healthcare’s unique requirements, from HIPAA compliance to EHR integration. We build production-ready NLP solutions that work reliably in real clinical environments.
Our healthcare AI specialists have developed clinical documentation systems, medical entity recognition models, and telemedicine platform integrations. We combine deep technical expertise with practical understanding of clinical workflows to deliver solutions that clinicians actually adopt and use.
Ready to explore NLP for your telemedicine platform? Schedule a free consultation with our healthcare AI team. We will assess your requirements, discuss implementation approaches, and provide a tailored roadmap for achieving your clinical and operational goals.
Frequently Asked Questions on NLP in Telemedicine
1. What is NLP in telemedicine, and how does it improve patient care?
NLP in telemedicine uses artificial intelligence to process and understand clinical language from virtual consultations, patient messages, and medical documentation. It improves patient care by reducing documentation burden on clinicians, enabling faster response to patient communications, and surfacing relevant clinical information during encounters. Clinicians spend more time on direct patient interaction and less on administrative tasks.
2. How accurate is NLP for medical documentation?
Accuracy varies by use case and implementation. Well-implemented clinical NLP systems achieve high accuracy for tasks like entity extraction and coding suggestions, though performance depends on the quality of training data and the complexity of the clinical content. Organizations should establish accuracy thresholds appropriate for each use case and implement human review workflows for clinical applications.
3. Is NLP in telemedicine HIPAA compliant?
NLP technology itself is neither compliant nor non-compliant. Compliance depends on how the technology is implemented and operated. Organizations must ensure appropriate technical safeguards, business associate agreements with vendors, access controls, audit logging, and data handling procedures. Both cloud-based and on-premise NLP deployments can be made HIPAA compliant with proper implementation.
4. What is the cost of implementing NLP in a telehealth platform?
NLP implementation costs vary significantly based on scope, approach, and existing infrastructure. Commercial NLP platforms typically involve subscription fees based on usage volume. Custom development requires upfront investment in data preparation, model development, and integration. Organizations should also budget for ongoing maintenance, monitoring, and model refinement. A phased approach starting with a focused use case helps manage costs while proving value.
5. How long does it take to implement NLP in telemedicine?
Implementation timelines range from weeks to months, depending on the approach. Integrating commercial NLP solutions with existing platforms may take 8 to 16 weeks for initial deployment. Custom model development adds time for data preparation and training. Pilot programs typically precede full rollout to validate performance and refine workflows. Organizations should plan for iterative improvement rather than expecting perfect results immediately.
6. Can NLP handle multiple languages in telemedicine applications?
Multilingual NLP is available but varies in capability across languages. English language medical NLP is the most mature, with other major languages increasingly supported. Organizations serving multilingual populations should evaluate language coverage as part of vendor selection. Some organizations deploy separate NLP models for different languages and use translation services to bridge gaps.
7. What is the difference between NLP and generative AI in healthcare?
NLP encompasses a broad range of language technologies, including entity extraction, classification, and analysis. Generative AI specifically focuses on creating new content like clinical summaries, patient communications, or documentation drafts. Modern healthcare AI often combines both capabilities. NLP extracts and structures information while generative AI produces human-readable outputs. Both require validation and oversight in clinical settings.
Need NLP Expertise for Telemedicine?
What to read next