- What Is Generative AI in Healthcare?
- Six Key Advantages of Generative AI in Healthcare
- Understanding Generative AI Healthcare Applications: 10 Real-World Use Cases
- 1. Ambient clinical documentation and auto-scribe
- 2. Medical imaging analysis and diagnostic enhancement
- 3. Clinical decision support and risk prediction
- 4. Drug discovery and accelerated development
- 5. Personalized medicine and treatment planning
- 6. Virtual nursing assistants and patient engagement
- 7. Synthetic data generation for research
- 8. Medical coding and billing automation
- 9. Medical literature analysis and research synthesis
- 10. Patient triage and care pathway optimization
- How to Implement Generative AI in Healthcare: A Practical Roadmap
- Key Challenges in Implementing Generative AI in Healthcare
- Partner with Space-O AI to Develop Secure and Scalable Healthcare Gen AI Systems
- Frequently Asked Questions About Generative AI in Healthcare
- Is generative AI ready for clinical use today?
- Will Generative AI replace doctors?
- What’s the average ROI timeline for generative AI in healthcare implementation today?
- What does a typical healthcare generative AI implementation cost?
- How do generative AI healthcare solutions handle patient privacy?
- How long does it take to implement Gen AI in healthcare solutions?
- How serious is the risk of bias in healthcare AI models?
- Which healthcare specialties see the strongest impact from AI?
Generative AI in Healthcare: What It Is, How It Works, and Why It Matters
Generative AI is rapidly becoming one of the most transformative technologies in healthcare. From automating clinical documentation to accelerating drug discovery and enhancing diagnostic accuracy, it is reshaping how providers, researchers, and healthtech companies deliver care.
As per a McKinsey survey, 85 percent of healthcare organizations are now either exploring or actively adopting generative AI, highlighting just how quickly the technology is moving from experimentation to real-world implementation.
As hospitals face rising workloads, operational inefficiencies, and increasing pressure to improve patient outcomes, generative AI offers a smarter and more scalable way to work with complex healthcare data. In our experience as a leading generative AI development company, we’re seeing a significant rise in healthcare organizations adopting gen AI across their everyday operations.
In this guide, we break down what generative AI really means for the healthcare sector, how it works, the most impactful use cases, and what organizations can expect as they adopt it. Learn about the benefits, challenges, and real-world applications of generative AI in healthcare.
What Is Generative AI in Healthcare?
Generative AI in healthcare refers to advanced AI models that can understand, analyze, and create new information based on large datasets. Instead of simply identifying patterns, generative AI produces outputs such as clinical notes, medical images, drug molecule designs, patient summaries, and risk predictions.
Building a generative AI model allows healthcare providers, researchers, and healthtech companies to automate manual tasks, accelerate decision-making, and deliver more personalized care. Generative AI models are trained on vast volumes of medical data such as EHR records, imaging datasets, clinical guidelines, and research literature.
Once trained, they can generate insights and content that support clinical workflows, administrative processes, and patient engagement.
Example: How Generative AI Works in a Real Healthcare Setting
Imagine a patient arrives at the emergency department with chest pain. The clinician needs to quickly review the patient’s history, analyze test results, document the visit, and decide on the next steps.
With generative AI:
- The system instantly summarizes the patient’s history, including past cardiac events, medications, and key lab results.
- It analyzes the ECG and chest X-ray, highlighting abnormalities and offering clinical insights.
- It auto-drafts the clinical note in real time as the examination progresses.
- It provides predictive risk analysis, showing the likelihood of complications based on similar cases.
Within minutes, the clinician has a complete, accurate view of the patient’s condition and can make quicker, more informed decisions.
Now that you understand how GenAI processes healthcare data, let’s explore the measurable benefits organizations are already realizing across clinical, operational, and financial dimensions.
Six Key Advantages of Generative AI in Healthcare
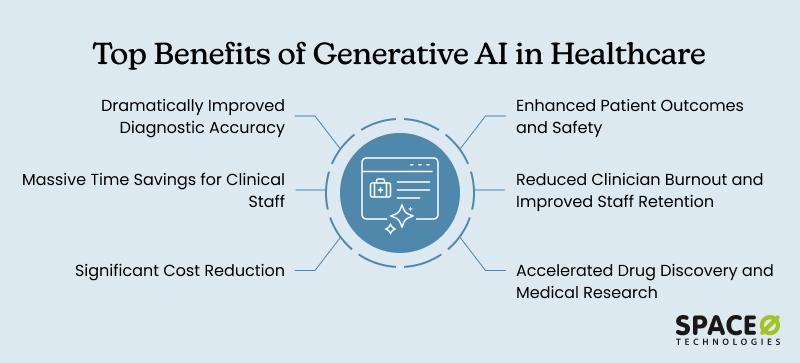
From reducing administrative burden to improving diagnostic accuracy and accelerating research, generative AI helps providers work more efficiently while delivering higher-quality patient care. Here are the core benefits of implementing gen AI in healthcare:
1. Improves diagnostic accuracy
AI maintains consistent performance without fatigue, detecting abnormalities humans miss during repetitive tasks. This consistency eliminates fatigue-related errors that cascade through treatment pathways. Early detection enables intervention when treatment is most effective, improving patient safety and transforming clinical outcomes significantly.
2. Saves time for clinical staff
Physicians redirect reclaimed documentation time to patient interaction and complex decision-making. Reduced administrative burden translates directly to capacity increases without hiring additional staff. Clinicians gain mental energy for better decisions, enabling treatment of more patients while improving care quality overall.
3. Reduces operational costs
Initial GenAI implementations fund larger initiatives through quick wins. Lower costs per patient enable treating more patients while improving efficiency and raising margins. Better outcomes reduce complications and readmissions. For healthcare organizations facing margin pressure, GenAI improves outcomes while simultaneously reducing costs.
4. Enhance patient outcomes and safety
GenAI prevents medication errors through automation and personalized treatment selection. AI-assisted surgery reduces complications while early detection enables intervention before terminal stages. Risk prediction supports preventive care. These capabilities translate to lives saved, suffering reduced, and improved quality of life across populations.
5. Reduces clinician burnout and improves staff retention
Automating administrative tasks transforms job satisfaction by letting clinicians work at peak expertise. Reduced burden improves retention, which is less expensive than recruiting new staff. Better care results from satisfied clinicians. Rural hospitals gain specialist access, enabling complex cases locally rather than requiring transport.
6. Accelerates drug discovery and medical research
GenAI compresses development timelines and reduces costs significantly, providing treatment access to terminal patients. Rare disease research becomes economically viable. Literature analysis and synthetic data generation accelerate progress across all fields. Research is completed in months versus years when data access improves and manual work is automated.
These benefits translate into real-world impact through specific applications. Here are ten proven use cases where healthcare organizations are deploying GenAI successfully today.
These benefits translate into real-world impact through specific applications. Here are ten proven use cases where healthcare organizations are deploying GenAI successfully today.
Build a Gen AI Solution That Drives Impact
Ready to convert the benefits of Gen AI into measurable ROI? Partner with Space-O AI to develop high-performing AI tools designed for your healthcare environment.Understanding Generative AI Healthcare Applications: 10 Real-World Use Cases
Generative AI is already making a measurable impact across hospitals, clinics, and healthtech platforms. Its ability to understand medical data, automate documentation, interpret images, and generate clinical insights is helping healthcare teams work faster and more accurately.
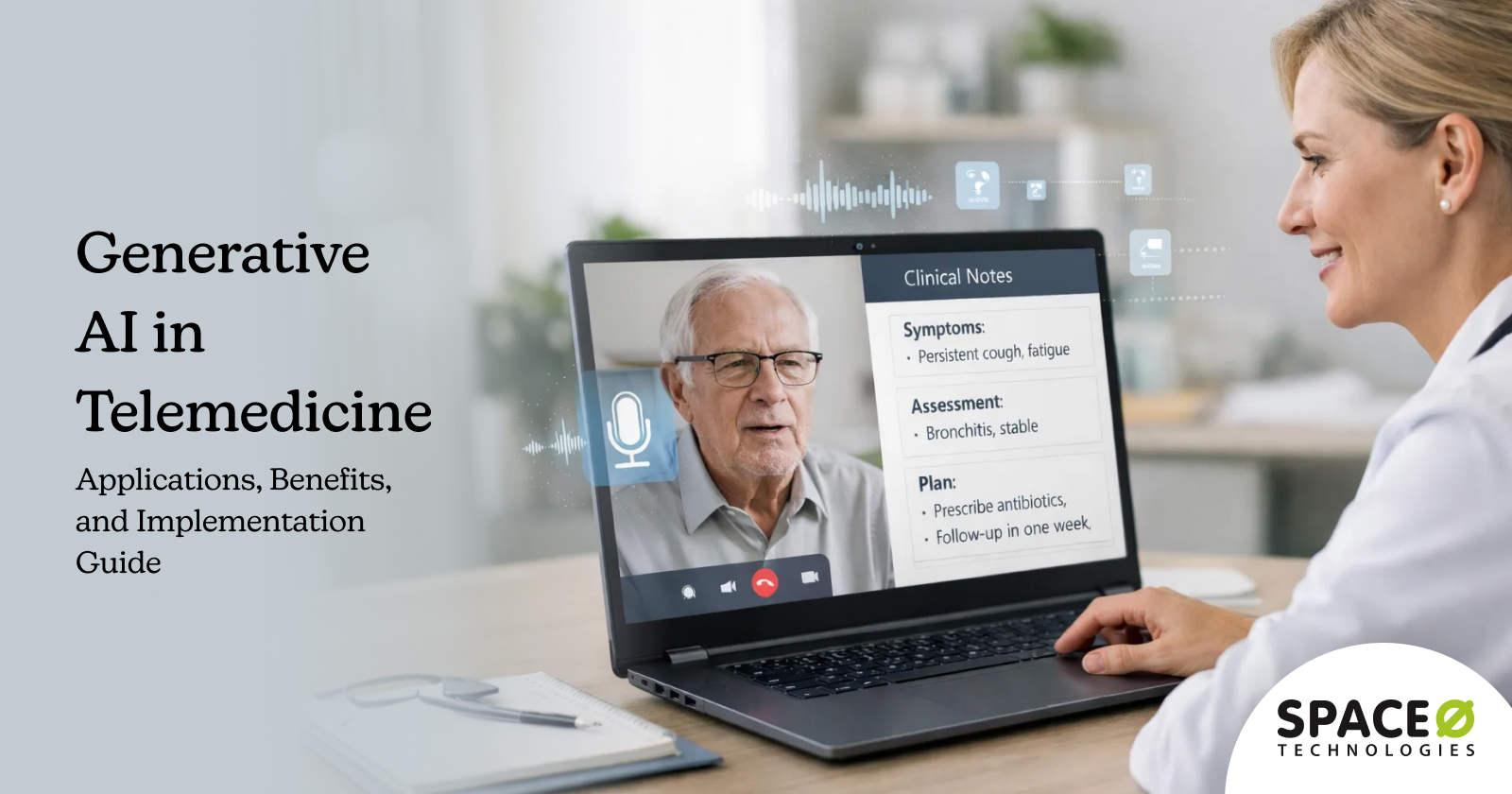
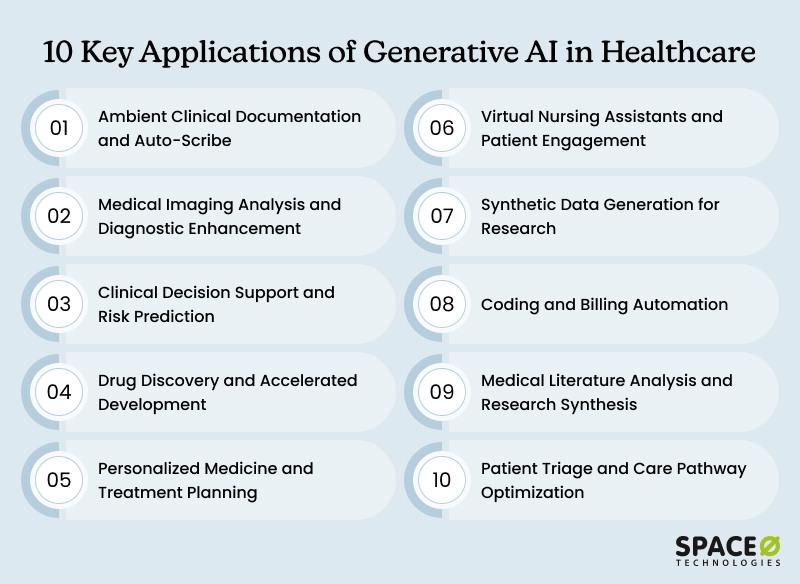
1. Ambient clinical documentation and auto-scribe
The problem
Physicians spend hours daily on documentation. Notes must be detailed enough for billing, legal defense, and care continuity. But they’re not patient care. They’re administrative requirements that pull clinicians away from patients, contribute to burnout, and consume the resource hospitals can least afford to lose: physician time.
The GenAI solution
Ambient documentation systems use natural language processing to listen to patient-provider conversations. The AI generates clinical notes in real-time, capturing history, assessment, and plan without requiring physicians to stop and type.
The impact
An NPJ study found that AI systems can reduce time documentation vt 20-30%, with some reporting after-hours work reduction up to 30%. Kaiser Permanente deployed this across 40 hospitals and 600+ medical offices, representing the largest generative AI healthcare implementation to date. Studies show physicians report improved focus on patient interaction and reduced stress.
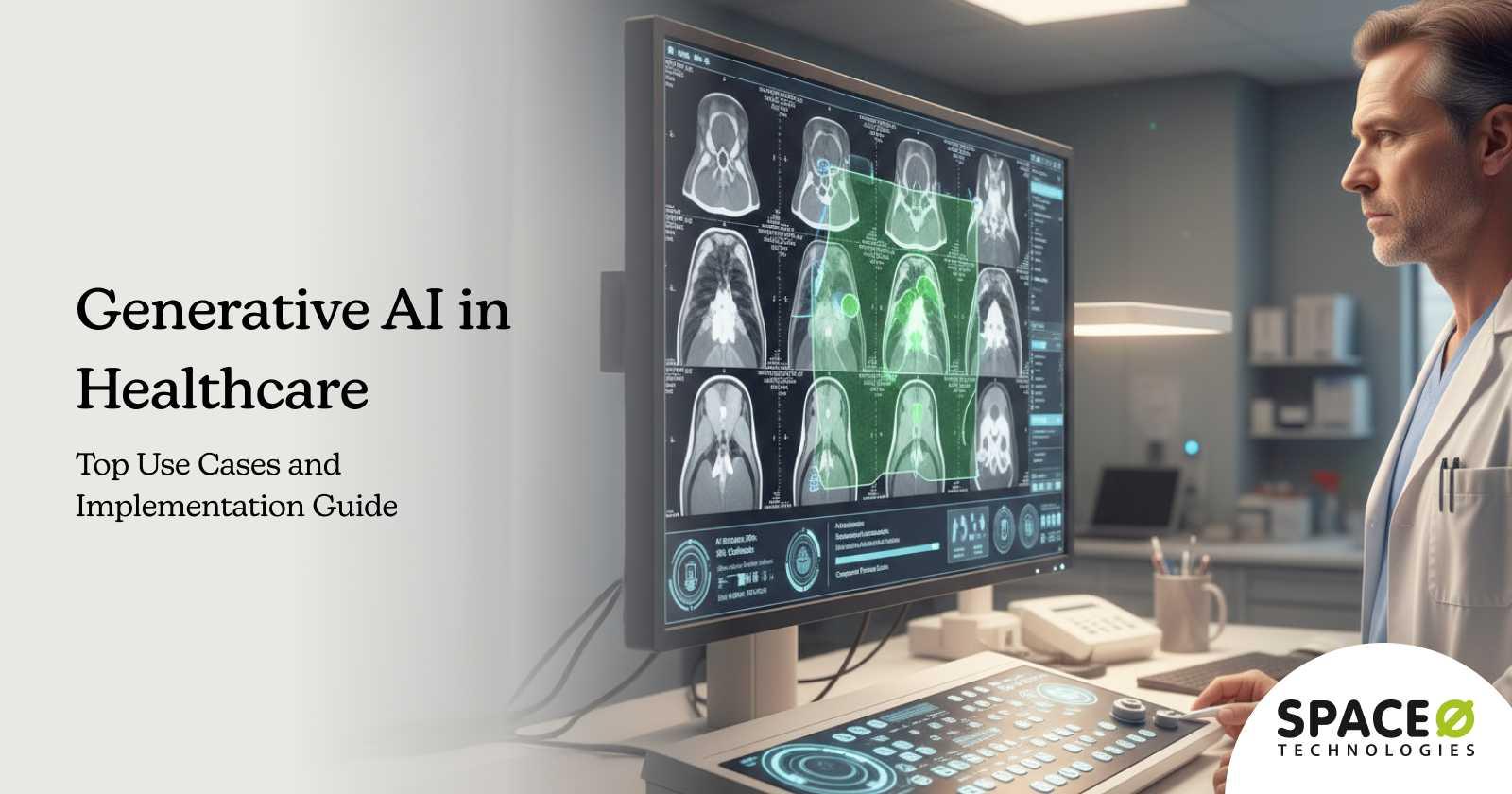
2. Medical imaging analysis and diagnostic enhancement
The challenge
Radiologists move through hundreds of images each day, and fatigue is unavoidable. When focus slips, even subtle abnormalities can be missed, allowing early cancers to hide in plain sight. The result? Patients wait weeks for reports, pushing treatment timelines further out.
The GenAI solution
AI models analyze medical images with consistency that humans can’t maintain. They enhance image quality by removing noise and improving clarity. They flag suspicious areas for radiologist review and compare current scans to historical images to identify changes.
The impact
An NPJ report states AI reduces radiologist workload by approximately 27% through concurrent assistance and pre-screening. AI diagnostic performance varies by application type, with recent meta-analyses showing sensitivity and specificity comparable to or exceeding healthcare professionals in multiple imaging domains.
Early-stage condition detection improves significantly, enabling intervention when treatment is most effective.
3. Clinical decision support and risk prediction
The challenge
Clinicians face complex cases requiring rapid decisions. They need current research evidence, patient history context, risk factors, and treatment success rates. Manual literature review takes hours. Memory has limits.
The GenAI solution
AI systems analyze patient data and compare it against clinical literature, research databases, and outcomes from similar patients. They recommend evidence-based treatment pathways, identify drug interaction risks, and predict patient deterioration before it becomes critical.
The impact
Improved diagnostic accuracy through evidence-based guidance. Better treatment selection reduces complications and adverse reactions. Early risk detection enables preventive interventions. A Yorkshire study found AI risk prediction models correctly identified patients needing hospital transfer in 80% of cases, without bias from clinician fatigue or experience level.
4. Drug discovery and accelerated development
The challenge
Drug discovery takes years of research and costs pharmaceutical companies and healthcare researchers billions to develop. Researchers manually screen millions of compounds. Clinical trials require years to complete. Most compounds fail. Patients waiting for breakthrough treatments may not live long enough to benefit.
The GenAI solution
GenAI systems rapidly generate novel drug compounds, predict their molecular interactions with disease targets, simulate their effects, and identify the most promising candidates for clinical testing. They accelerate clinical trial design by matching patients to trials efficiently and predicting treatment responses.
The impact
A Pharmacological Reviews report states that AI-discovered molecules achieve 80–90% Phase I success rates versus 40–65% historically. AI reduces discovery costs by 40% and compresses timelines from five years to 12-18 months, enabling investment in rare diseases.
Pro tip: Building a drug discovery AI solution requires specialized expertise in molecular biology, computational chemistry, and machine learning. Hire generative AI engineers with pharma domain knowledge for better outcomes, as the technical complexity is too high for general developers.
5. Personalized medicine and treatment planning
The challenge
Healthcare traditionally treats disease types, not individual patients. Patients with the same diagnosis receive the same protocols. But genetic variations, lifestyle factors, comorbidities, and medication interactions mean identical treatment produces different outcomes.
The GenAI solution
Personalized medicine using GenAI analyzes individual patient genetics, medical history, biomarkers, and lifestyle factors. It recommends customized treatment plans tailored to how that specific patient’s biology will likely respond. For rare genetic disorders, it assists in diagnosis by analyzing facial recognition and genetic data.
The impact
Better treatment selection reduces medication failures and adverse reactions. Patients experience fewer side effects and better outcomes. Particularly powerful for cancer treatment, where tumor genetics directly guide therapy selection.
6. Virtual nursing assistants and patient engagement
The challenge
Patients want access to healthcare information 24/7. Many have routine questions that don’t need a physician’s time. Patient self-care improves with education and reminders. But healthcare systems can’t staff 24/7 phone lines.
The GenAI solution
AI chatbots powered by large language models handle routine patient inquiries, medication reminders, health education, and symptom tracking. They operate in multiple languages, across web, mobile, and messaging platforms. For routine issues, they resolve problems immediately. For complex issues, they escalate to human clinicians.
The impact
Significant potential for healthcare sector savings through virtual nursing assistance. Patients get answers immediately rather than waiting. 24/7 availability. Reduced call volume to human staff. Improved patient engagement and medication compliance through reminders and education.
7. Synthetic data generation for research
The challenge
Healthcare research requires large, diverse datasets. Real patient data is limited, especially for rare diseases. Privacy regulations restrict data sharing. Researchers can’t access sufficient data to train models.
The GenAI solution
Generative AI creates realistic, fully anonymized synthetic patient data. These datasets preserve statistical properties of real data without containing actual patient information. Researchers can access diverse datasets without privacy violations.
The impact
Research accelerates when diverse training data becomes available. Rare disease research, previously impossible due to data scarcity now become feasible. Privacy concerns disappear when data is synthetic. Model training improves with augmented datasets.
8. Medical coding and billing automation
The challenge
Medical coders manually read clinical notes and assign diagnosis codes for billing. Coding errors cause claim denials. Hospitals lose significant revenue to coding mistakes, denials, and billing errors.
The GenAI solution
GenAI systems read clinical notes, automatically identify and code diagnoses and procedures, and flag potential denial risks. Human coders review and validate before submission.
The impact
Revenue recovery through reduced errors. Faster billing cycle. Reduced coding staff burnout (coding is repetitive and detail-intensive). Immediate ROI as recovered revenue begins flowing within months.
9. Medical literature analysis and research synthesis
The challenge
Medical research volume is overwhelming. Thousands of papers are published daily. Researchers manually sorting literature for patterns and insights waste months.
The GenAI solution
GenAI systems analyze thousands of research papers, identify patterns, extract key findings, and synthesize insights across studies. They accelerate literature reviews from months to days.
The impact
Research progresses faster. Researchers identify gaps and validate hypotheses quickly. Cross-study patterns become visible. An analysis that would take months of manual work can be completed in days.
10. Patient triage and care pathway optimization
The challenge
Emergency departments triage patients to determine priority. Nurses assess hundreds of patients. Incorrect triage means critical patients wait, or non-urgent cases consume resources.
The GenAI solution
AI systems evaluate patient symptoms, vital signs, medical history, and current presentations. They recommend care pathways and triage priority based on evidence and pattern recognition.
The impact
Better triage accuracy ensures urgent patients receive rapid treatment. Hospital readmission rates show improvement with optimized care pathways. Time spent reviewing patients decreases substantially with decision support. Huma’s AI platform demonstrated significant improvements across multiple health systems, validated through clinical implementation.
While these use cases show how generative AI can transform healthcare operations and patient care, successful adoption requires following a systematic implementation process. Let’s look at the key steps in implementing generative AI technology in healthcare.
Build a Gen AI Solution Designed for Your Healthcare Use Case
Whether you need clinical note generation, medical image analysis, predictive insights, or patient engagement automation, we design Gen AI systems that fit your exact use case.How to Implement Generative AI in Healthcare: A Practical Roadmap
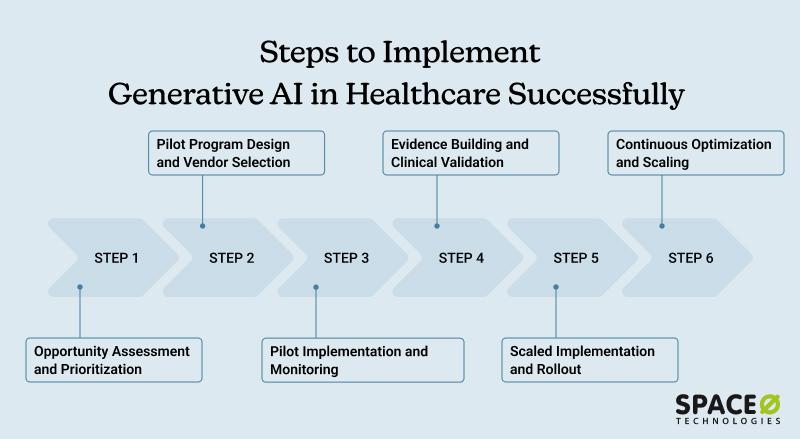
Successful deployment of generative AI for healthcare follows a structured, phased approach that builds evidence, demonstrates value, and scales progressively. Working with specialized Gen AI development partners accelerates this roadmap and transforms strategy into action more efficiently.
Phase 1: Opportunity assessment and prioritization
Identify where applications of generative AI in healthcare create the highest impact. Map workflows consuming the most time or generating the most errors. Where would faster decision-making create the most value?
Quantify the impact of solving each problem. If administrative automation saves $2M annually, that’s a high priority. If documentation automation frees 2 hours per clinician daily, that’s high impact. Build a prioritized opportunity list ranked by ROI and implementation complexity.
Tip: most organizations overestimate easy wins and miss bigger opportunities. That’s where generative AI consulting service providers add value, identifying the gaps you’d otherwise overlook.
Key activities
- Conduct workflow analysis across departments
- Interview clinicians and administrators about pain points
- Benchmark against industry standards
- Assess organizational readiness: data infrastructure, system integration capabilities, clinician buy-in, budget availability, executive sponsorship
Phase 2: Pilot program design and vendor selection
Choose a focused, high-impact use case. Don’t attempt enterprise-wide transformation in phase one. Select one clinical department or service line with executive champions willing to pilot Gen AI in healthcare solutions.
Here, you have two options: custom-develop your generative AI healthcare solution for your organization or buy a ready-to-use SaaS healthcare platform. The former option yields better output as your platform is developed based on your unique requirements and use cases. You can partner with a healthcare AI development company to build your healthcare gen AI platform.
Key activities
- Evaluate 3-5 potential vendors thoroughly
- Request detailed proposals and cost estimates
- Conduct reference calls with similar healthcare organizations
- Negotiate contracts with clear success criteria and exit clauses
- Establish governance structure and decision-making authority
Phase 3: Pilot implementation and monitoring
Deploy in controlled environments with active monitoring. Run AI in parallel with existing processes initially; AI provides recommendations while clinicians make decisions unchanged. This preserves patient safety while gathering performance evidence.
Track performance metrics continuously. Monitor for accuracy degradation, unexpected behaviors, or adverse events. Gather clinician feedback weekly and address frustrations quickly. Document what works, what doesn’t, and what needs adjustment.
Key activities
- Configure systems for your specific workflows
- Train initial user cohorts intensively
- Establish daily standup meetings to address issues
- Monitor key performance indicators in real-time dashboards
- Document all findings and lessons learned
Phase 4: Evidence building and clinical validation
Measure rigorously. Does the AI perform as promised? Are clinicians adopting it? Is it creating expected value? Document outcomes, complications, and any adverse events meticulously.
Validate performance across patient populations. Test edge cases where AI might struggle. Verify consistency across diverse clinical scenarios, not just impressive performance on best-case examples.
Key activities
- Conduct rigorous statistical analysis of pilot data
- Present results to clinical leadership and medical staff committees
- Prepare case studies and success stories
- Begin planning for scaled deployment based on pilot learnings
Phase 5: Scaled implementation and rollout
Based on pilot success, expand to additional departments, facilities, or use cases. Maintain the same governance, monitoring, and feedback loops at scale. Train staff comprehensively. Create standard operating procedures. Establish escalation pathways for edge cases.
Monitor performance post-deployment. Continuously retrain models as organizational practices evolve and new patient populations or conditions emerge.
Key activities
- Develop a detailed rollout timeline and communication plan
- Train super-users in each department to support peers
- Create comprehensive documentation and standard operating procedures
- Establish ongoing model monitoring and retraining cadence
- Schedule regular check-ins to assess adoption and ROI achievement
Phase 6: Continuous optimization and scaling
Generative AI healthcare solutions mature over time with proper governance. Monitor model performance continuously. Collect user feedback systematically. Identify new opportunities for Gen AI use cases in healthcare expansion based on pilot successes.
Invest in advanced analytics to understand ROI across different departments and use cases. Build internal expertise so your team becomes less dependent on external vendors. Plan for next-generation implementations leveraging learnings from initial deployments.
Key activities
- Establish an AI governance committee with clinical and technical representation
- Implement model monitoring dashboards with alerts for performance issues
- Conduct quarterly business reviews to assess ROI and optimization opportunities
- Build organizational AI literacy through ongoing education programs
- Identify and prioritize next-wave AI initiatives
With a clear implementation roadmap in place, you now understand how generative artificial intelligence moves from concept to operational reality in healthcare settings. However, implementing generative AI isn’t always a straightforward path. It is important to consider common implementation challenges and roadblocks and prepare for them beforehand.
Need Help Implementing Gen AI in Your Healthcare System?
Our AI experts guide you through data preparation, model selection, integration, security, and compliance to ensure a smooth and successful implementation.Key Challenges in Implementing Generative AI in Healthcare
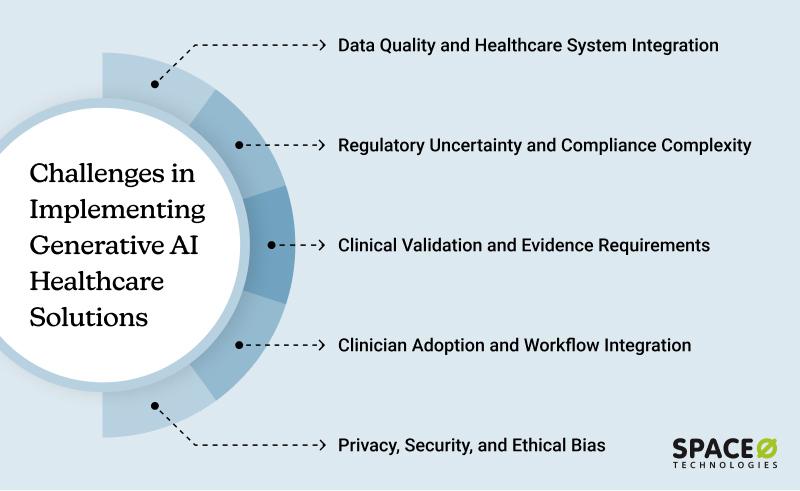
Moving generative AI and healthcare from promising pilot to full-scale operations reveals consistent implementation obstacles. Understanding these challenges upfront enables smarter planning, better resource allocation, and effective risk mitigation strategies.
1. Data quality and healthcare system integration
The problem
Healthcare data lives in fragmented silos. Patient records span multiple EHR systems with inconsistent formatting. Some data is structured (diagnoses, procedures), much is unstructured (clinical notes written in free text).
Compliance regulations restrict data sharing between systems. Generative AI in medicine requires clean, standardized, representative data from diverse patient populations and clinical scenarios.
Solution
- Invest in data governance before generative AI integration implementation
- Build data pipelines that continuously feed clean, standardized data to AI models
- Use synthetic data augmentation to address population gaps and rare conditions
- Partner with an experienced generative AI integration company with knowledge of healthcare data integration
- Conduct data quality audits and establish ongoing monitoring dashboards
- Implement master data management (MDM) solutions to standardize formats across systems
2. Regulatory uncertainty and compliance complexity
The problem
FDA oversight in healthcare AI is evolving rapidly. There’s no universally clear regulatory pathway for many applications. Liability questions remain unresolved: if an AI-assisted diagnosis is wrong, who bears responsibility?
Solution
- Begin with use cases where regulatory clarity exists (administrative automation, documentation support)
- Engage the FDA early through pre-submission meetings for clinical applications
- Implement rigorous validation protocols before clinical deployment
- Maintain detailed audit trails of AI recommendations and clinician decisions
- Include clear liability provisions and insurance coverage in vendor contracts
- Work with legal counsel specializing in healthcare AI regulation
- Document compliance with HIPAA, state privacy laws, and industry standards
3. Clinical validation and evidence requirements
The problem
Before widespread adoption, generative AI and healthcare systems must demonstrate safety, efficacy, and reliability through rigorous validation studies. This requires careful study design, statistical analysis, and sometimes peer-reviewed publication. The validation process is lengthy and expensive, slowing deployment.
Solution
- Conduct parallel pilots where AI runs alongside existing processes without changing clinical decisions
- Gather performance evidence over weeks or months before scaling
- Test across multiple sites and diverse patient populations before declaring success
- Collaborate with academic medical centers on validation studies to accelerate evidence generation
- Publish results in peer-reviewed journals to build clinical community confidence
- Establish clear success metrics and realistic accuracy expectations upfront
- Plan for continuous monitoring post-deployment to identify performance drift
4. Clinician adoption and workflow integration
The problem
Physicians are often skeptical of AI tools. If implementation feels clunky or disrupts existing workflows, clinicians abandon tools and revert to old processes. Without clinician buy-in, even excellent AI fails through non-use.
Solution
- Involve clinicians in design from day one, not after system development
- Ensure generative AI in healthcare examples integrate smoothly into existing workflows without adding complexity
- Provide thorough training tailored to different user roles
- Establish ongoing support channels and feedback mechanisms
- Celebrate early wins visibly so colleagues hear about success stories
- Create clinical champion programs where respected clinicians evangelize adoption
- Measure and share utilization metrics and user satisfaction regularly
- Rapidly implement clinician feedback to demonstrate responsiveness
5. Privacy, security, and ethical bias
The problem
AI requires patient data, raising legitimate privacy concerns. Large language models can memorize and regurgitate individual patient information if not carefully designed. Algorithms trained on historical healthcare data can perpetuate or amplify existing disparities, leading to worse outcomes for underrepresented populations.
Solution
- Implement differential privacy techniques that prevent the extraction of individual records
- Use federated learning, where models train locally without centralizing sensitive data
- Audit algorithms for bias across demographic groups before and after deployment
- Ensure training data represents all populations where AI will operate
- Prioritize model explainability so you understand why AI made each recommendation
- Conduct regular security audits and penetration testing
- Establish ethics oversight committees beyond just technical review
- Maintain clear data usage policies and obtain informed patient consent
With these challenges understood and mitigation strategies in place, you’re ready to move forward with implementing generative AI use cases in healthcare at your organization. The next section provides a structured roadmap for turning these insights into action.
Partner with Space-O AI to Develop Secure and Scalable Healthcare Gen AI Systems
Generative AI is rapidly reshaping the healthcare landscape, enabling providers to deliver faster diagnoses, personalized care, streamlined operations, and more accurate decision-making. As adoption accelerates across hospitals, diagnostics, pharma, and digital health startups, organizations are increasingly turning to Gen AI to drive efficiency, improve patient experiences, and reduce clinical overhead.
But unlocking these benefits requires the right technical expertise, seamless integration, and a deep understanding of healthcare workflows and compliance needs.
This is where Space-O AI becomes your trusted AI development partner. Backed by 15+ years of AI engineering experience and 500+ successful AI projects, we help healthcare companies build secure, accurate, and scalable Gen AI solutions tailored to real-world use cases.
Whether you need a custom large language model, a clinical co-pilot, AI-enabled automation, or a fully integrated patient experience solution, our team ensures every project is delivered with precision, quality, and compliance.
Check our portfolio to see how we’ve helped global healthcare organizations transform operations through intelligent AI systems.
AI Recruiting Software
An end-to-end AI recruitment platform was built by our team to automate interviews using ChatGPT and Whisper. It generates questions, transcribes candidate responses, evaluates answers, and reduces hiring time by up to 90%, helping teams make fair, faster, data-backed hiring decisions.
Fine-tuning Stable Diffusion XL
We fine-tuned Stable Diffusion XL using LoRA and DreamBooth to produce consistent, high-quality custom visuals from just a few reference images. Our optimized training pipeline reduced compute requirements while enabling precise style replication, allowing clients to generate personalized images with exceptional accuracy and efficiency.
AI Document Analyzer & QA System
For a US-based church, Space-O created an AI-powered document ingestion and chatbot tool. Uploaded content is processed into a searchable knowledge base, enabling the chatbot to instantly answer member questions using context-aware responses derived from church documentation.
If you are ready to bring responsible, high-impact Gen AI into your healthcare ecosystem, Space-O AI has the experience, technology, and expertise to make it happen. Schedule a free consultation with our AI experts today and start your healthcare AI implementation journey.
Frequently Asked Questions About Generative AI in Healthcare
Is generative AI ready for clinical use today?
Yes, in specific applications. Successful generative AI in healthcare examples include ambient documentation, medical coding automation, and imaging analysis support, all proven and deployed in production at major health systems. These lower-risk use cases, where clinical pathways are established, show measurable ROI today.
Other applications, like primary diagnosis support, are still developing. Start with proven use cases, gather evidence, then expand after clinical validation demonstrates safety and efficacy.
Will Generative AI replace doctors?
No. Healthcare workers will remain central to patient care. Healthcare is fundamentally about human connection, judgment, and complex decision-making. AI eliminates repetitive administrative work and augments clinician decision-making, not replaces them.
The shift: physicians freed from documentation and routine analysis focus on complex cases, patient relationships, teaching, and research. The work becomes more fulfilling. Physicians using AI most effectively report greater job satisfaction, not displacement fears.
What’s the average ROI timeline for generative AI in healthcare implementation today?
Most organizations achieve positive ROI within 12-18 months, generating $3-4 return per $1 invested. However, timelines vary by use case.
Administrative automation (coding, prior auth, and scheduling) shows returns in 3-9 months. Clinical documentation support delivers ROI in 6-12 months. Drug discovery applications may take 18-36 months but deliver larger returns once scaled. Variation reflects implementation complexity and value realization mechanisms.
What does a typical healthcare generative AI implementation cost?
Pilot projects typically range $50K-$150K. Full facility deployments span $200K-$1M+. Variation reflects scope, complexity, and scale.
Ongoing costs run 15-20% of the initial investment annually for maintenance, retraining, infrastructure, and support. Most organizations recover implementation costs within 12-18 months through labor savings, error reduction, and improved efficiency. Choose use cases with clear, quantifiable ROI before committing.
How do generative AI healthcare solutions handle patient privacy?
Privacy concerns are legitimate but manageable. Modern approaches include differential privacy (algorithmic noise preventing individual record extraction), federated learning (local model training without centralizing data), data minimization, access controls, encryption, and de-identification.
The key is choosing vendors implementing these safeguards and verifying compliance through security audits.
How long does it take to implement Gen AI in healthcare solutions?
Initial assessment to scaled deployment typically takes 6-12 months for straightforward use cases, 12-24 months for complex ones.
Timeline breakdown: assessment 4-8 weeks, vendor selection 6-12 weeks, pilot deployment 8-16 weeks, clinical validation 8-12 weeks, scaled rollout 12-24 weeks. Phased approaches allow organizations to learn and demonstrate incremental value before major commitments.
How serious is the risk of bias in healthcare AI models?
Bias is a significant concern across the AI in healthcare industry. If AI models learn from data reflecting historical disparities, they can reinforce unequal outcomes. Reducing this risk requires diverse datasets, routine bias audits, explainable recommendations, and ongoing monitoring. These safeguards help ensure the future of AI in healthcare remains fair, safe, and clinically reliable.
Which healthcare specialties see the strongest impact from AI?
Administrative tasks benefit widely, but some specialties see exceptional gains. Radiology and pathology lead due to their image-heavy workflows. Oncology, cardiology, emergency medicine, and primary care also see strong returns from risk prediction, triage, and documentation support. These patterns signal where the future of AI in healthcare is headed within a rapidly evolving AI in healthcare industry.
Build Your Healthcare Gen AI Solution With Our Experts
What to read next