- What Is a Virtual AI Telemedicine Assistant?
- Key Features of AI Virtual Assistants for Telemedicine
- Benefits of AI Virtual Assistants in Telemedicine
- AI Virtual Assistant Development Process for Telemedicine
- Challenges in AI Virtual Assistant Development for Telemedicine and How to Overcome Them
- AI Virtual Assistant Development Cost for Telemedicine
- Real-World Use Cases of AI Virtual Assistants in Telemedicine
- Space-O AI — Your Trusted Partner for Telemedicine AI Virtual Assistant Development
- Frequently Asked Questions
- 1. What is the difference between an AI virtual assistant and a healthcare chatbot?
- 2. How long does it take to develop an AI virtual assistant for telemedicine?
- 3. Is it possible to make AI virtual assistants HIPAA-compliant?
- 4. Can AI virtual assistants integrate with existing EHR systems?
- 5. What technologies power AI virtual assistants for healthcare?
- 6. How do AI virtual assistants handle medical emergencies?
- 7. What is the cost of maintaining an AI virtual assistant after launch?
Building an AI Telemedicine Virtual Assistant: A Complete Guide
Telemedicine has improved access to care, but virtual healthcare delivery still faces challenges such as clinician overload, delayed patient responses, and fragmented communication. As patient volumes continue to grow, healthcare organizations need intelligent automation to maintain care quality without increasing operational strain.
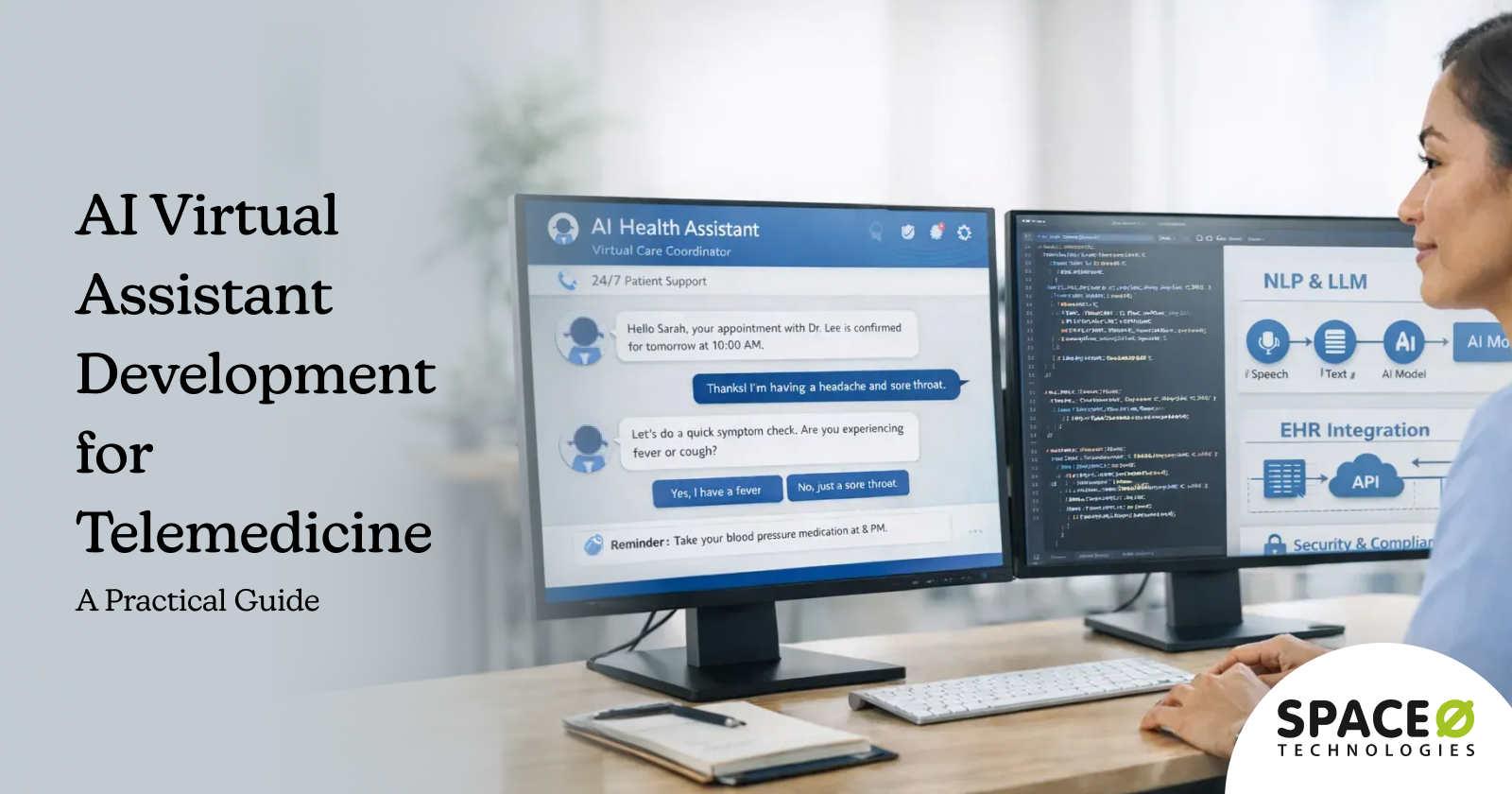
AI virtual assistants in telemedicine address these challenges by automating patient interactions, supporting clinicians, and streamlining workflows across the virtual care journey. Powered by NLP and machine learning, these assistants can understand patient queries, guide symptom intake, schedule appointments, provide follow-up instructions, and assist clinicians with documentation and triage.
The rapid adoption of virtual assistants reflects their growing role in healthcare. According to Grand View Research, the global healthcare virtual assistant market is expected to reach USD 455.27 billion by 2030, highlighting how healthcare providers and digital health companies are investing in AI-driven assistance to scale telemedicine services efficiently.
From patient-facing chatbots to clinician support assistants, AI virtual assistants are becoming a core component of modern telemedicine platforms.
In this blog, we explore how AI virtual assistants work in telemedicine, key use cases, benefits, development process, and cost considerations. Drawing from our experience as a leading AI healthcare development agency, we have shared expert insights on how to build secure, compliant, and scalable virtual assistant solutions.
What Is a Virtual AI Telemedicine Assistant?
A telemedicine AI virtual assistant is an intelligent, software-based assistant designed to support patients and healthcare providers throughout the virtual care journey. It uses artificial intelligence technologies such as natural language processing, machine learning, and conversational AI to understand user inputs, respond in natural language, and perform healthcare-specific tasks within telemedicine platforms.
For patients, AI virtual assistants act as the first point of interaction in virtual care. They can answer common health-related questions, guide symptom intake, schedule or reschedule appointments, send reminders, and provide post-consultation instructions. By handling routine interactions, the assistant improves response times and ensures patients receive timely support without waiting for human intervention.
For clinicians and care teams, telemedicine AI virtual assistants support workflow automation and decision support. They can summarize virtual visit conversations, extract key clinical details, assist with documentation, flag urgent cases, and route patients to the appropriate care pathway. When integrated with EHR systems, these assistants help reduce administrative workload while maintaining accuracy and compliance.
Virtual telemedicine assistant vs telemedicine chatbot
Developing a virtual telemedicine assistant is not the same as developing a telemedicine chatbot. A virtual assistant offers superior intelligence, better diagnostic capabilities, and helps deliver excellent patient care. Here’s how these two approaches are different:
| Aspect | Telemedicine Virtual Assistant | Telemedicine Chatbot |
| Primary Role | End-to-end support across patient and clinician workflows | Handles predefined patient queries and basic interactions |
| Intelligence Level | Advanced AI with NLP, context awareness, and decision support | Rule-based or limited NLP with scripted responses |
| Conversation Depth | Multi-turn, contextual conversations across sessions | Single-session or linear conversations |
| Use Case Scope | Symptom intake, triage, documentation support, care coordination, follow-ups | FAQs, appointment booking, basic symptom questions |
| Clinical Support | Assists clinicians with summaries, alerts, and workflow automation | No clinician-facing intelligence |
| Decision-Making | Can prioritize cases and recommend next steps with guardrails | No prioritization or clinical reasoning |
| Personalization | Learns from patient history and interaction context | Minimal personalization |
| Compliance Readiness | Built with healthcare-grade security and compliance controls | Often requires customization for compliance |
| Scalability | Designed for enterprise-scale telemedicine platforms | Suitable for simple, high-volume interactions |
Now that we understand what virtual assistants are, let us explore the specific features that make them effective in telemedicine settings.
Key Features of AI Virtual Assistants for Telemedicine
Selecting the right features determines whether your virtual assistant delivers meaningful value or becomes another underutilized technology investment. Features typically fall into two categories: essential capabilities for foundational functionality and advanced features for comprehensive patient engagement.
1. Essential features for telemedicine virtual assistants
Essential features form the foundation of any healthcare virtual assistant. These capabilities address core patient needs and admtinistrative workflows, making them ideal for developing a telemedicine MVP or organizations beginning their AI journey. Most healthcare providers can launch a functional virtual assistant with these features within 3-4 months.
| Feature | Description |
| Text-based chat interface | Web and mobile chat enabling patients to ask questions and receive instant responses |
| Appointment scheduling | Self-service booking with real-time provider availability and calendar integration |
| Patient registration | Digital intake forms collecting demographics, insurance, and medical history |
| Appointment reminders | Automated SMS, email, and push notifications for upcoming visits |
| FAQ responses | Instant answers to common questions about services, hours, and procedures |
| Basic symptom collection | Structured questionnaires gathering pre-visit health information |
| Provider routing | Intelligent direction of patients to appropriate care teams or specialists |
| Medication reminders | Scheduled notifications supporting prescription adherence |
| HIPAA-compliant storage | Secure data handling meets healthcare regulatory requirements |
| Basic encryption | Data protection for all transmissions and stored information |
These essential features enable healthcare organizations to automate routine tasks, reduce front-desk workload, and provide basic 24/7 patient support without requiring significant infrastructure changes.
2. Advanced features for telemedicine virtual assistants
Advanced features transform virtual assistants from simple automation tools into intelligent healthcare partners. These capabilities leverage sophisticated AI, deeper system integrations, and personalized engagement strategies to deliver superior clinical and operational outcomes. Organizations typically add these features after validating their MVP with real users.
| Feature | Description |
| Voice-enabled interactions | Natural speech recognition and conversational responses for hands-free use |
| Multi-language support | Real-time translation serving diverse patient populations |
| AI-powered triage | Risk stratification and urgency assessment using clinical algorithms |
| Sentiment analysis | Detection of patient emotions to adjust tone and escalate when needed |
| Personalized health recommendations | Tailored advice based on patient history, conditions, and preferences |
| Biometric data interpretation | Analysis of wearable device data including vitals and activity levels |
| Multi-EHR integration | Connections with multiple electronic health record systems |
| Proactive health nudges | Preventive care reminders and wellness tips based on patient profiles |
| Chronic care check-ins | Automated daily monitoring for diabetes, hypertension, and other conditions |
| Patient history summarization | AI-generated summaries for providers and patients |
Advanced features significantly enhance patient satisfaction and clinical outcomes but require additional development time, specialized AI expertise, and robust integration architecture. Many of these capabilities, including sentiment analysis, personalized recommendations, and patient history summarization, are powered by generative AI development technologies that continue to evolve rapidly.
3. Multi-modal interaction capabilities
Modern virtual assistants support multiple interaction channels to meet patients where they are. Text-based interfaces work well for detailed inquiries, while voice enables hands-free interaction for elderly patients or those with accessibility needs. These conversational capabilities are built on LLM development foundations that enable natural language understanding across channels.
Visual interfaces help present lab results, medication schedules, and health trends in easily digestible formats. SMS integration extends reach to patients without smartphone apps.
With a clear understanding of essential and advanced features, let us examine the benefits these virtual assistants deliver to healthcare organizations.
Need Help Choosing a Feature Set for Your AI Telemedicine Assistant?
Our healthcare AI experts help you prioritize features that deliver maximum ROI. Get a free consultation to define your virtual assistant roadmap.
Benefits of AI Virtual Assistants in Telemedicine
Implementing AI virtual assistants delivers measurable improvements across patient experience, clinical efficiency, and operational costs. Healthcare organizations investing in these solutions report significant returns within the first year of deployment.
1. 24/7 patient availability
Virtual assistants provide round-the-clock support, answering patient queries and handling appointments without requiring human staff. This constant availability significantly improves patient satisfaction and ensures care access regardless of time zones or office hours.
2. Reduced administrative burden
AI handles repetitive tasks like scheduling, intake forms, and insurance verification, freeing clinical staff to focus on direct patient care. Administrative teams can redirect their efforts toward complex cases requiring human judgment and empathy.
3. Improved patient engagement
Proactive health reminders, personalized recommendations, and consistent follow-ups increase patient adherence to treatment plans. Engaged patients demonstrate better health outcomes, fewer missed appointments, and higher satisfaction scores.
4. Scalability without proportional costs
Healthcare organizations handle increasing patient volumes without linear headcount growth. Virtual assistants manage thousands of simultaneous conversations, enabling practices to expand services without proportionally increasing administrative staff.
5. Multilingual support
Virtual assistants serve diverse patient populations with multi-language capabilities, breaking down language barriers that often prevent effective care delivery. This accessibility improves health equity across communities.
6. Data-driven insights
Every patient interaction generates valuable data about preferences, concerns, and behaviors. Analytics dashboards help administrators identify trends, optimize services, and make evidence-based decisions about resource allocation.
These benefits compound over time as virtual assistants learn from interactions and organizations refine their deployment strategies. Organizations considering these solutions can benefit from AI consulting services to assess readiness and define implementation roadmaps. Now, let us explore the development process for building these solutions.
AI Virtual Assistant Development Process for Telemedicine
Building an effective healthcare virtual assistant requires a structured approach that balances technical excellence with clinical accuracy and regulatory compliance. The following five-step process ensures successful development from concept to deployment.
Step 1: Requirements analysis and use case definition
Every successful virtual assistant project begins with thorough requirements gathering. This phase identifies who will use the system, what problems it will solve, and how it will integrate with existing workflows.
Rushed requirements lead to costly rework and underperforming solutions. Organizations without in-house expertise often hire AI consultants to guide this critical discovery phase.
Action items
- Identify target user personas, including patients, clinicians, and administrative staff
- Define primary use cases and map conversation flows for each scenario
- Assess compliance requirements, including HIPAA, state regulations, and organizational policies
- Evaluate the existing system landscape for integration points with EHR, scheduling, and billing
- Establish success metrics and KPIs for measuring deployment effectiveness
Step 2: Technology stack selection
Choosing the right AI technology stack ensures scalability, performance, and long-term maintainability. Healthcare virtual assistants require specialized considerations around security, accuracy, and integration capabilities that consumer applications do not face.
Action items
- Select NLP and LLM frameworks such as GPT-4, Claude, or domain-specific fine-tuned models
- Choose voice recognition technology if supporting speech-based interactions
- Determine a cloud infrastructure provider with healthcare compliance certifications
- Plan database architecture for HIPAA-compliant data storage and retrieval
- Evaluate integration middleware for connecting with healthcare systems
Step 3: Design conversational architecture
Conversation design shapes patient experience more than any other factor. Poorly designed flows frustrate users and increase abandonment rates. Effective design anticipates patient needs, handles errors gracefully, and maintains natural dialogue progression.
Action items
- Map detailed conversation flows and decision trees for each use case
- Design intent recognition models and entity extraction for medical terminology
- Create fallback responses and escalation pathways for unhandled scenarios
- Develop personality guidelines ensuring a consistent, empathetic tone
- Build error recovery mechanisms that guide patients back to productive paths
Step 4: Integration development
Healthcare virtual assistants derive much of their value from seamless integration with clinical and administrative systems. Isolated chatbots that cannot access patient records or update appointments provide limited utility compared to fully integrated solutions.
You can partner with a professional AI integration agency like Space-O AI to ensure smooth connectivity with existing healthcare infrastructure.
Action items
- Implement EHR/EMR connections using HL7 FHIR interoperability standards
- Connect calendar and scheduling systems for real-time availability
- Integrate payment processing for copays and billing inquiries
- Link pharmacy systems for prescription refills and interaction checks
- Establish wearable device data feeds for biometric monitoring
Step 5: Testing, validation, and deployment
Rigorous testing protects patient safety and ensures regulatory compliance. Healthcare AI requires additional validation steps beyond standard software testing, including clinical accuracy verification and security audits.
Action items
- Conduct clinical accuracy testing with a healthcare professional review
- Perform comprehensive security assessments and penetration testing
- Execute user acceptance testing with representative patient populations
- Complete HIPAA compliance audits and documentation
- Deploy with monitoring dashboards and feedback collection mechanisms
Following this structured process significantly increases project success rates. However, development teams must also prepare for common challenges, which we explore next.
Build Your AI Telemedicine Assistant With Space-O AI — 15+ Years of AI Engineering Expertise
Space-O AI has delivered 500+ AI projects with seamless healthcare integrations. Schedule a call to discuss your development requirements and timeline.
Challenges in AI Virtual Assistant Development for Telemedicine and How to Overcome Them
Building healthcare virtual assistants presents unique challenges that development teams must anticipate and address. Understanding these obstacles helps organizations plan effectively and avoid costly missteps.
Challenge 1: HIPAA compliance and data security
Healthcare virtual assistants handle protected health information (PHI), including medical histories, symptoms, and treatment details. HIPAA regulations impose strict requirements for data handling, storage, and transmission. Non-compliance risks significant fines and reputational damage.
Solution
- Implement end-to-end encryption for all data transmissions between patients and systems
- Use HIPAA-compliant cloud infrastructure with signed Business Associate Agreements
- Deploy role-based access controls, limiting data visibility to authorized personnel
- Maintain comprehensive audit logs tracking all PHI access and modifications
- Conduct regular security assessments and third-party penetration testing
Challenge 2: Medical accuracy and liability
AI responses must be medically accurate to avoid patient harm. Virtual assistants providing incorrect health information can lead to delayed treatment, inappropriate self-care, or dangerous drug interactions. Legal liability concerns require careful risk management.
Solution
- Implement human-in-the-loop review for any clinical recommendations or triage decisions
- Use evidence-based medical knowledge bases validated by clinical experts
- Include clear disclaimers distinguishing AI assistance from professional medical advice
- Design escalation pathways ensuring rapid connection to human providers when needed
- Conduct ongoing clinical validation with healthcare professionals reviewing AI outputs
Challenge 3: EHR integration complexity
Healthcare organizations use diverse EHR platforms with varying data formats, APIs, and security requirements. Epic, Cerner, Meditech, and other systems each require specific integration approaches. This complexity extends development timelines and increases costs.
Solution
- Adopt healthcare interoperability standards, particularly HL7 FHIR, for data exchange
- Partner with EHR vendors or certified integration specialists with proven experience
- Build a modular architecture supporting connections to multiple EHR systems
- Plan comprehensive data mapping and normalization workflows for consistent information
- Allocate sufficient time and budget for integration testing and troubleshooting
Challenge 4: Patient trust and adoption
Patients may hesitate to share sensitive health information with AI systems or prefer human interaction for medical concerns. Low adoption undermines ROI and limits the benefits organizations can achieve from their investment.
Solution
- Design transparent AI that clearly explains its capabilities and limitations to users
- Provide easy, obvious escalation paths to human support at any conversation point
- Implement empathetic conversation design that acknowledges patient concerns
- Gather continuous feedback and visibly improve based on user suggestions
- Communicate privacy protections clearly to build confidence in data handling
Challenge 5: Finding skilled AI development talent
Building healthcare virtual assistants requires specialized expertise spanning conversational AI, healthcare compliance, clinical workflows, and system integration. Finding developers with this combination of skills proves difficult, and training generalist developers takes considerable time.
Solution
- Partner with experienced AI development companies with proven track records
- Consider hiring dedicated AI developers with healthcare domain experience
- Build cross-functional teams combining AI engineers, healthcare consultants, and compliance experts
- Invest in ongoing training to keep teams current with rapidly evolving AI technologies
- Establish knowledge transfer processes to reduce dependency on individual team members
Successfully navigating these challenges requires experienced development partners and realistic project planning. Understanding costs helps organizations budget appropriately.
AI Virtual Assistant Development Cost for Telemedicine
AI virtual assistant development costs vary significantly based on feature complexity, integration requirements, compliance needs, and team location. Healthcare organizations must budget not only for initial development but also for ongoing maintenance, infrastructure, and continuous improvement.
Understanding the telemedicine solution development cost structure helps decision-makers set realistic expectations and compare vendor proposals effectively. The following breakdown reflects typical project scopes based on industry standards.
| Development Stage | Basic Virtual Assistant | Advanced Virtual Assistant |
| MVP Development | $50,000 – $100,000 | $100,000 – $200,000 |
| Full Platform | $150,000 – $250,000 | $250,000 – $500,000+ |
| Integration Costs | $20,000 – $50,000 | $50,000 – $150,000 |
| Annual Maintenance | $30,000 – $60,000 | $60,000 – $120,000 |
Breakdown of each category
MVP development covers the initial build of core functionality. Basic MVPs include text-based chat, appointment scheduling, FAQ handling, and single EHR integration. Advanced MVPs add voice capabilities, AI-powered triage, multi-language support, and more sophisticated conversational flows requiring additional NLP engineering.
Full Platform costs represent comprehensive production systems with complete feature sets. Basic platforms handle standard patient interactions across web and mobile channels. Advanced platforms include multi-EHR integrations, predictive analytics, chronic care management modules, and sophisticated personalization engines.
Integration costs depend heavily on existing infrastructure complexity. Basic integrations connect to single EHR systems and standard scheduling platforms using established APIs. Advanced integrations span multiple EHRs, pharmacy systems, wearable devices, billing platforms, and custom legacy systems requiring specialized middleware development.
Annual maintenance covers ongoing operational needs. Basic maintenance includes hosting, security patches, minor updates, and standard support. Advanced maintenance adds continuous AI model improvement, expanded feature development, dedicated support teams, and proactive performance optimization.
Key factors that impact the development cost
- Number of use cases and conversation complexity requiring development
- Voice capabilities versus text-only interactions
- Number of EHR and third-party system integrations required
- Compliance and security requirements beyond baseline HIPAA
- Multi-language support for diverse patient populations
- Custom AI model training versus pre-built LLM implementations
- Ongoing cloud infrastructure and API usage costs
ROI consideration: Healthcare organizations typically recover their investment through reduced administrative costs, improved patient throughput, decreased no-show rates, and better staff utilization. Organizations report significant reductions in routine inquiry handling costs within the first year.
Want an Accurate Cost Estimate for Your Healthcare Virtual Assistant Project?
Our team provides detailed project assessments with transparent pricing. Get a customized quote based on your specific features and integration needs.
Real-World Use Cases of AI Virtual Assistants in Telemedicine
AI virtual assistants deliver value across diverse healthcare scenarios. Understanding proven use cases helps organizations identify high-impact starting points for their implementations.
1. Patient intake and triage automation
Virtual assistants streamline the pre-visit process by collecting symptoms, medical history, and insurance information before appointments. AI-powered triage assesses urgency and routes patients to appropriate care levels, whether emergency services, same-day appointments, or scheduled visits. This automation reduces wait times, improves throughput, and ensures patients receive timely care.
2. Chronic disease management
Patients with diabetes, hypertension, heart conditions, and other chronic diseases benefit from daily virtual check-ins. Assistants collect blood glucose readings, blood pressure measurements, and symptom updates, alerting care teams when values fall outside acceptable ranges. Medication adherence reminders and lifestyle coaching support better disease control between provider visits.
3. Mental health support
Virtual assistants provide 24/7 emotional support, crisis detection, and therapy reinforcement. They deliver cognitive behavioral therapy exercises, track mood patterns, and remind patients about counseling homework. When detecting concerning language or escalating distress, assistants immediately connect patients with human counselors or crisis services. Mental health represents one of the fastest-growing telehealth segments, creating strong demand for scalable support solutions.
4. Post-discharge follow-up
Hospital readmissions cost healthcare systems significantly and indicate care quality gaps. Virtual assistants conduct automated check-ins after discharge, monitoring medication adherence, symptom progression, and recovery milestones. Early identification of complications enables intervention before conditions worsen, reducing emergency department visits and improving patient outcomes.
5. Elderly patient care
Senior patients often struggle with complex healthcare navigation and medication management. Virtual assistants designed for elderly users feature simplified interfaces, larger text, voice-first interactions, and patient repetition of instructions. Family caregiver notifications keep loved ones informed about appointments, medication schedules, and health status changes.
These use cases demonstrate the versatility of AI virtual assistants across patient populations and clinical scenarios. Organizations often start with one or two high-impact use cases before expanding functionality.
Space-O AI — Your Trusted Partner for Telemedicine AI Virtual Assistant Development
AI virtual assistants transform telemedicine by automating patient intake, scheduling, triage, and follow-up care. With the right development approach, healthcare organizations achieve 24/7 availability, reduced administrative burden, and measurably improved patient outcomes.
Space-O AI brings 15 years of software development expertise with 500+ successful AI projects developed and delivered worldwide. Our team specializes in building HIPAA-compliant, production-ready AI solutions that integrate seamlessly with existing healthcare infrastructure and workflows.
Our 80+ AI development specialists have built intelligent healthcare assistants using cutting-edge LLMs, NLP, and voice technologies. We deliver enterprise-grade virtual assistants with proven EHR integrations, robust security controls, and measurable ROI for healthcare organizations.
Ready to build an AI virtual assistant for your telemedicine platform? Schedule a free consultation with our healthcare AI experts today. We will analyze your requirements and create a detailed development roadmap tailored to your specific needs.
Frequently Asked Questions
1. What is the difference between an AI virtual assistant and a healthcare chatbot?
AI virtual assistants are more sophisticated than chatbots, offering contextual understanding, multi-modal interactions including voice and text, proactive patient engagement, and continuous learning from interactions. Chatbots typically follow predefined rules and scripts with limited flexibility.
2. How long does it take to develop an AI virtual assistant for telemedicine?
MVP development typically takes 3-6 months, covering core features and basic integrations. Full-featured virtual assistants with comprehensive EHR integrations, voice capabilities, and advanced AI may require 6-12 months, depending on complexity and compliance requirements.
3. Is it possible to make AI virtual assistants HIPAA-compliant?
Yes, AI virtual assistants can achieve full HIPAA compliance through proper encryption, access controls, audit logging, secure cloud infrastructure with signed BAAs, staff training, and documented policies. Compliance requires ongoing monitoring and regular assessments.
4. Can AI virtual assistants integrate with existing EHR systems?
Yes, modern virtual assistants integrate with EHR systems using healthcare interoperability standards like HL7 FHIR. Integration enables real-time access to patient records, appointment scheduling, clinical documentation, and care plan updates.
5. What technologies power AI virtual assistants for healthcare?
Key technologies include large language models such as GPT-4 and Claude, natural language processing frameworks, speech recognition engines, machine learning for personalization, and healthcare APIs for system integrations. Cloud platforms provide scalable infrastructure.
6. How do AI virtual assistants handle medical emergencies?
Virtual assistants are programmed to recognize emergency indicators through keyword detection and sentiment analysis. Upon detecting emergencies, they immediately provide emergency contact information, offer to connect with crisis services, and escalate to human providers. Clear disclaimers emphasize they do not replace emergency care.
7. What is the cost of maintaining an AI virtual assistant after launch?
Annual maintenance typically ranges from $30,000 to $120,000, depending on complexity. Costs cover cloud infrastructure, AI model updates, security monitoring, compliance audits, bug fixes, and continuous improvement based on user feedback and changing requirements.
Build Your Healthcare Virtual Assistant
What to read next



