- What Is Computer Vision in Telemedicine?
- Key Applications of Computer Vision in Telemedicine
- Benefits of Computer Vision for Telehealth Providers
- How Computer Vision Systems Work in Telehealth Platforms
- Challenges in Implementing Computer Vision for Telemedicine
- Computer Vision Telemedicine Development: Cost and Timeline
- Best Practices for Implementing Computer Vision in Your Telehealth Platform
- The Future of Computer Vision in Telehealth
- Partner with Space-O AI for Computer Vision in Telemedicine
- Frequently Asked Questions
- 1. What is computer vision in telemedicine, and how does it work?
- 2. What are the main applications of computer vision in telehealth?
- 3. How accurate is AI-powered medical image analysis?
- 4. Is computer vision for telemedicine HIPAA compliant?
- 5. How much does it cost to implement computer vision in a telehealth platform?
- 6. What are the regulatory requirements for medical computer vision systems?
- 7. Can computer vision replace radiologists and other specialists?
Computer Vision in Telemedicine: Applications, Benefits, and Implementation Guide
Telemedicine has expanded access to healthcare, but virtual care often lacks the visual context clinicians rely on during in-person examinations. Limited visibility can make it harder to assess symptoms, track disease progression, or validate patient-reported information during remote consultations.
Computer vision bridges this gap by enabling AI systems to analyze images and video captured through cameras, mobile devices, and connected medical equipment. By interpreting visual data such as skin images, wound photos, facial expressions, posture, and movement, computer vision helps clinicians make more informed decisions during virtual care encounters.
The growing adoption of visual AI in healthcare reflects its increasing importance. According to Precedence Research, the AI in the telemedicine market reached $26.11 billion in 2025 and is projected to grow to $176.94 billion by 2034. This rapid growth highlights how technologies like computer vision are becoming foundational to next-generation telemedicine platforms.
As telemedicine platforms mature, visual AI capabilities are becoming essential for improving diagnostic accuracy, remote monitoring, and patient engagement.
In this blog, we explore how computer vision works in telemedicine, key use cases, benefits, implementation costs, and adoption best practices. We have shared expert tips and insights as a trusted computer vision development company to help you implement computer vision-based intelligence into your telemedicine platform.
What Is Computer Vision in Telemedicine?
Computer vision in telemedicine refers to AI systems that analyze medical images, video feeds, and visual patient data to support remote diagnosis, monitoring, and clinical decision-making. These systems extract clinically relevant information from visual inputs that would traditionally require in-person examination or specialist interpretation.
Unlike basic image viewing in telehealth platforms, computer vision applies deep learning algorithms to detect patterns, classify conditions, segment anatomical structures, and track changes over time. The technology bridges the gap between what clinicians can observe through a screen and what they could assess during physical examination.
The following table outlines the core computer vision tasks used in telemedicine applications.
| CV Task | Description | Telemedicine Application |
| Image Classification | Categorizing images into predefined classes | Skin lesion classification, disease presence detection |
| Object Detection | Locating and identifying specific objects | Tumor localization, anatomical landmark identification |
| Semantic Segmentation | Pixel-level classification of image regions | Wound area measurement, organ boundary delineation |
| Instance Segmentation | Distinguishing individual objects of the same class | Cell counting in pathology, multiple lesion tracking |
| Temporal Video Analysis | Analyzing patterns across video frames | Respiratory rate monitoring, movement assessment |
These tasks rely on sophisticated deep learning architectures that have matured significantly over the past decade.
The following deep learning architectures power most medical computer vision applications.
| Architecture | Strength | Best For |
| Convolutional Neural Networks (CNNs) | Extracting hierarchical features from visual data | General medical image classification and detection |
| U-Net | Precise boundary delineation with limited training data | Medical image segmentation tasks |
| Vision Transformers | Capturing long-range dependencies in images | Complex pattern recognition across large image areas |
| ResNet Variants | Training very deep networks without degradation | High-accuracy complex diagnostic tasks |
For organizations beginning their AI software development journey, understanding these architectural foundations helps in evaluating vendor capabilities and making informed technology decisions.
The real value of computer vision emerges when these technologies address specific clinical workflows. Let us examine the key applications transforming telemedicine today.
Key Applications of Computer Vision in Telemedicine
Computer vision enables capabilities that were previously impossible in remote care settings. A healthcare software development company building telehealth solutions can integrate these applications to dramatically expand diagnostic capabilities without requiring patients to visit physical facilities.
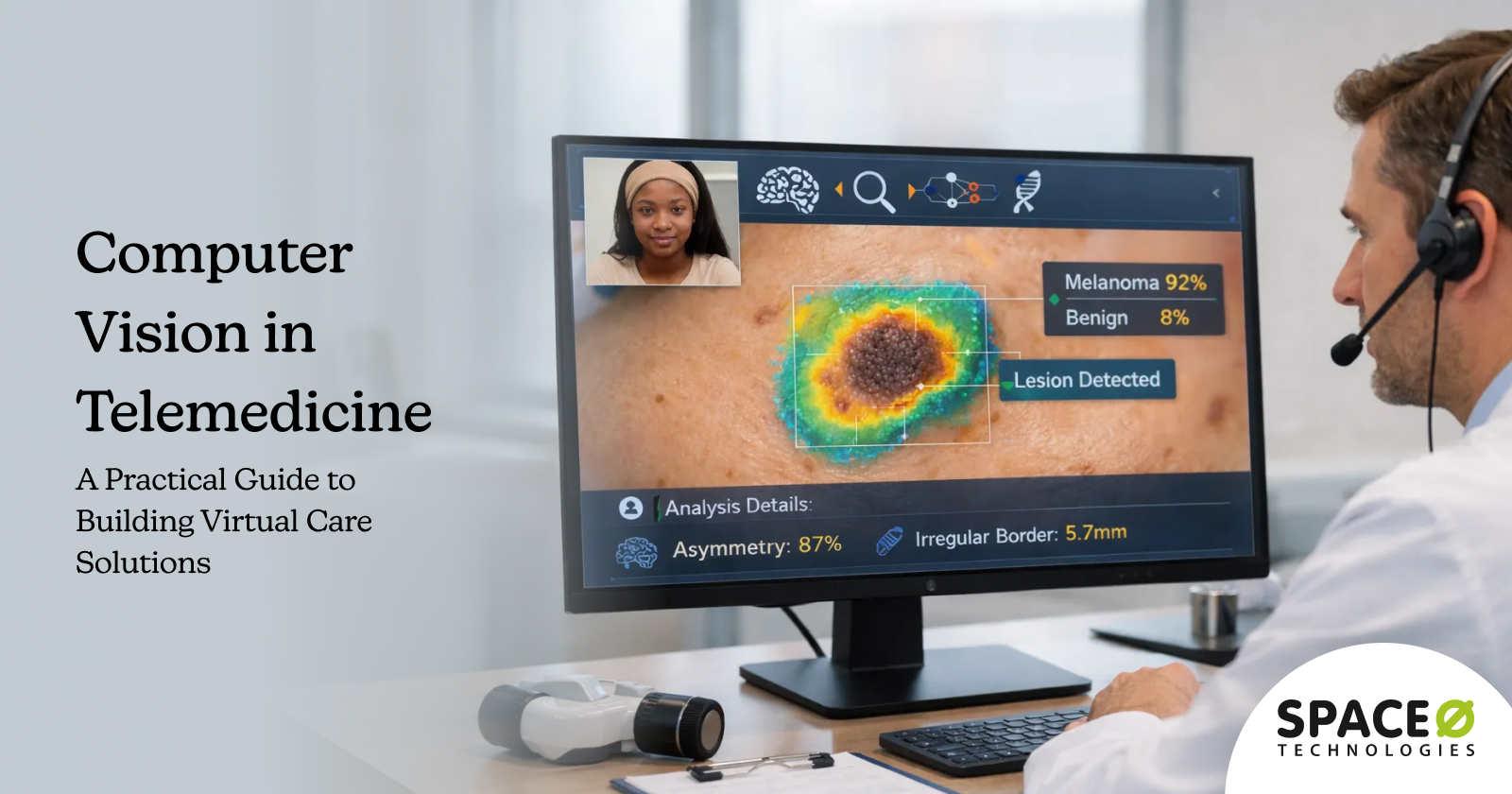
1. Dermatology and skin condition assessment
What it does: AI systems analyze smartphone-captured images to identify skin conditions, classify lesion types, and flag potential malignancies for specialist review.
Key capabilities:
- Melanoma and skin cancer detection with 90%+ sensitivity
- Inflammatory condition and infection diagnosis
- Chronic skin disease monitoring and progression tracking
Clinical impact: Faster diagnosis, reduced unnecessary referrals, and improved patient access to specialist expertise without in-person visits.
2. Ophthalmology and retinal imaging
What it does: Computer vision analyzes fundus photographs to detect diabetic retinopathy, glaucoma, and age-related macular degeneration through portable retinal cameras or smartphone attachments.
Key capabilities:
- Microaneurysm, hemorrhage, and exudate detection
- Automated severity grading per international standards
- Urgent referral identification for vision-threatening conditions
Clinical impact: Faster diagnosis, reduced unnecessary referrals, and improved patient access to specialist expertise without in-person visits.
3. Radiology image analysis
What it does: Computer vision pre-screens medical images, highlights suspicious regions, and prioritizes urgent cases for radiologist review across X-rays, CT scans, MRIs, and mammograms.
Key capabilities:
- Pneumonia and lung nodule detection in chest X-rays
- Stroke and trauma identification in CT scans
- Breast cancer screening support in mammography
Clinical impact: Faster diagnosis, reduced unnecessary referrals, and improved patient access to specialist expertise without in-person visits.
4. Physical therapy and movement analysis
What it does: Pose estimation algorithms assess patient movement, gait patterns, and exercise performance through standard video feeds during remote rehabilitation sessions.
Key capabilities:
- Joint angle and range of motion tracking
- Movement symmetry and compensation pattern detection
- Automated repetition counting and performance scoring
Clinical impact: Faster diagnosis, reduced unnecessary referrals, and improved patient access to specialist expertise without in-person visits.
5. Remote patient monitoring via video
What it does: Video-based algorithms extract physiological data from standard camera feeds, detecting vital signs and behavioral patterns without wearable devices.
Key capabilities:
- Contactless heart rate and respiratory rate measurement
- Facial expression and emotional state analysis
- Fall detection and emergency alerting for elderly patients
Clinical impact: Faster diagnosis, reduced unnecessary referrals, and improved patient access to specialist expertise without in-person visits.
6. Digital pathology
What it does: Computer vision analyzes digitized tissue samples for cancer detection, cell classification, and biomarker quantification across whole slide images containing billions of pixels.
Key capabilities:
- Mitotic figure counting and tumor margin measurement
- Cellular abnormality identification and classification
- Second opinion workflow support for rare conditions
Clinical impact: Faster diagnosis, reduced unnecessary referrals, and improved patient access to specialist expertise without in-person visits.
Understanding these applications reveals why healthcare organizations increasingly prioritize computer vision investments. The next section examines the specific benefits driving adoption.
Benefits of Computer Vision for Telehealth Providers
Computer vision delivers measurable improvements across clinical, operational, and financial dimensions. Each benefit compounds the value proposition for organizations investing in visual AI capabilities.
1. Improved diagnostic accuracy
AI-powered image analysis reduces missed diagnoses by consistently applying learned patterns across every case. Studies demonstrate computer vision matching specialist-level accuracy for specific conditions while eliminating variability from fatigue, distraction, or experience gaps that affect human readers.
2. Reduced diagnostic turnaround time
Automated pre-screening prioritizes urgent cases for immediate attention while routing routine findings through standard workflows. What previously required days for specialist review can be triaged within minutes, enabling faster treatment initiation for time-sensitive conditions.
3. Expanded specialist access
Remote image analysis connects patients in underserved areas with specialist expertise without travel burden. A rural clinic can obtain dermatology or ophthalmology consultations through AI-assisted telehealth rather than waiting months for specialist appointments in distant facilities.
4. Consistent quality assessment
Computer vision applies identical diagnostic criteria to every image, eliminating inter-observer variability that affects clinical outcomes. Quality metrics become measurable and improvable through systematic algorithm refinement across providers and locations.
5. Enhanced patient engagement
Visual progress tracking shows patients measurable improvement in wound healing, skin conditions, or rehabilitation performance. This tangible feedback motivates continued treatment compliance and strengthens the patient-provider relationship despite physical distance.
6. Operational efficiency gains
Automated analysis handles routine screening while clinicians focus on complex cases requiring human judgment. Organizations looking to build these capabilities can hire computer vision developers with healthcare AI expertise to accelerate implementation and multiply clinician capacity without proportional staffing increases.
These benefits materialize only through proper technical implementation. The following section explains how computer vision systems function within telehealth platforms.
Apply Computer Vision to Real Telemedicine Workflows
Space-O AI designs use case-driven computer vision models that fit seamlessly into telemedicine platforms.
How Computer Vision Systems Work in Telehealth Platforms
Implementing computer vision in telemedicine requires coordinated technical components spanning image acquisition, AI processing, and clinical integration. Understanding this architecture helps organizations plan implementations and evaluate vendor solutions.
Step 1: Image acquisition and preprocessing
Quality input data determines computer vision performance more than any algorithmic factor. Telemedicine applications must address image capture challenges that differ significantly from controlled clinical imaging environments.
1.1 Define camera and hardware requirements
Camera quality requirements vary by application. Dermatology assessment needs sufficient resolution to visualize fine skin texture and color variations. Retinal imaging requires specialized hardware attachments. Video-based vital signs monitoring demands consistent frame rates and adequate lighting.
1.2 Implement capture guidance systems
Real-time capture guidance helps patients and clinicians obtain usable images. On-screen prompts direct proper positioning, distance, and lighting while automated quality checks reject substandard captures before submission.
1.3 Apply preprocessing pipelines
Preprocessing standardizes images before AI analysis through these essential steps:
- Color normalization to account for lighting variations
- Resolution standardization across different capture devices
- Noise reduction while preserving clinically relevant details
- Anatomical alignment for consistent positioning
- Quality scoring to flag unusable images for recapture
Step 2: AI model processing
Trained deep learning models analyze preprocessed images to extract clinical insights. The processing pipeline varies by application but follows common patterns.
2.1 Extract visual features
Feature extraction identifies relevant visual patterns through convolutional layers that progressively abstract raw pixels into meaningful representations. These learned features capture edges, textures, shapes, and spatial relationships that distinguish normal from pathological findings.
2.2 Perform multi-condition analysis
Multi-pathology detection enables single images to be analyzed for multiple conditions simultaneously. A chest X-ray analysis might screen for pneumonia, cardiomegaly, pleural effusion, and lung nodules in one pass, maximizing the clinical value extracted from each image.
2.3 Generate confidence scores
Confidence scoring accompanies every prediction, indicating algorithm certainty. High-confidence findings route differently than borderline cases requiring additional review. Clinical thresholds balance sensitivity against specificity based on condition severity and downstream workflow implications.
Organizations building these capabilities benefit from experienced machine learning development partners who understand both the technical requirements and clinical validation processes.
Step 3: Clinical integration and workflow
Computer vision outputs must integrate seamlessly with existing clinical systems to deliver value. Standalone AI tools that disrupt workflows face adoption barriers regardless of technical performance.
3.1 Connect with EHR systems
EHR integration connects image analysis results with patient records. Findings, confidence scores, and supporting visualizations populate appropriate documentation fields. Historical comparisons become possible when current results link to prior imaging studies.
3.2 Design decision support interfaces
Clinician decision support interfaces present AI insights without overwhelming or misleading users. Effective designs highlight regions of interest on original images, explain algorithm reasoning where possible, and clearly communicate uncertainty.
3.3 Implement oversight mechanisms
Human-in-the-loop oversight mechanisms ensure appropriate clinical review for all AI-generated findings. Escalation pathways route uncertain or critical findings to qualified specialists. Audit trails document the decision process for quality assurance and medicolegal purposes.
Challenges in Implementing Computer Vision for Telemedicine
Despite compelling benefits, computer vision implementation in healthcare faces significant challenges. Successful projects anticipate these obstacles and design solutions from the outset.
1. Data quality and image standardization
Medical image quality varies dramatically across capture devices, environments, and operators. Patient-captured smartphone images present particular challenges with inconsistent lighting, blur, and framing that differ significantly from controlled clinical imaging environments.
Solutions
- Standardized capture protocols with visual guides and automated feedback
- Real-time quality assessment rejects unusable images before submission
- Data augmentation during training to improve robustness to variations
- Graceful degradation that flags low-confidence results rather than producing unreliable predictions
2. Regulatory compliance and FDA approval
Medical computer vision systems face regulatory scrutiny as Software as Medical Device (SaMD). The FDA and international regulators require evidence of safety and effectiveness before marketing AI diagnostic tools, with classification determining the regulatory burden and timeline.
Solutions
- Early regulatory strategy consultation before development begins
- Clinical validation studies designed to support regulatory submissions
- Quality management systems aligned with FDA expectations
- Post-market surveillance plans for ongoing safety monitoring
3. Technical infrastructure requirements
Computer vision demands substantial computational resources for both model training and inference. Healthcare organizations must plan infrastructure capable of handling image processing workloads while meeting performance, availability, and latency requirements for clinical workflows.
Solutions
- Cloud deployment leveraging healthcare-specific platforms with built-in compliance
- Edge computing for latency-sensitive applications and offline capability
- Model optimization techniques reduce computational requirements
- Scalable architectures handling variable workloads efficiently
4. Privacy and consent considerations
Medical images constitute protected health information requiring HIPAA-compliant handling throughout the computer vision pipeline. Patient consent, data security, and privacy preservation present ongoing challenges that must be addressed systematically across acquisition, processing, and storage.
Solutions
- HIPAA-compliant cloud platforms with Business Associate Agreements
- De-identification techniques, removing patient identifiers from images
- Federated learning enables model improvement without centralizing sensitive data
- Consent workflows integrated into image capture applications
5. Integration with legacy systems
Many healthcare organizations operate legacy EHR systems and clinical infrastructure that lack modern APIs. Integrating computer vision outputs with these systems requires custom development, middleware solutions, or phased modernization approaches that add complexity and cost.
Solutions
- HL7 FHIR adoption for standardized healthcare data exchange
- SolutionsMiddleware layers translating between modern AI systems and legacy infrastructure
- Phased integration, starting with standalone workflows before deep integration
- Vendor partnerships providing pre-built connectors for common EHR platforms
Understanding implementation challenges helps organizations budget appropriately. The following section provides realistic cost and timeline expectations.
Overcome Computer Vision Implementation Challenges With Confidence
Partner with Space-O AI to address accuracy, compliance, and scalability challenges in telemedicine AI.
Computer Vision Telemedicine Development: Cost and Timeline
Computer vision development for telemedicine typically ranges from $75,000 to $300,000+, depending on scope, complexity, and regulatory requirements. Organizations should budget for complete implementation, including data preparation, model development, integration, validation, and deployment, rather than focusing solely on algorithm development costs.
The following table breaks down costs by implementation complexity.
| Complexity Level | Typical Features | Cost Range | Timeline |
| Basic | Single imaging modality, classification task, web integration | $75,000–$120,000 | 4–6 months |
| Intermediate | Multiple modalities, segmentation capabilities, EHR integration, mobile support | $120,000–$200,000 | 6–9 months |
| Advanced | Full diagnostic suite, multi-pathology detection, edge deployment, regulatory submission | $200,000–$300,000+ | 9–14 months |
Several factors drive costs beyond basic development:
- Data preparation and annotation often consume 30–40% of project budgets. Medical images require expert labeling by clinicians, and sufficient training data may require partnerships with healthcare institutions or synthetic data generation.
- Regulatory compliance adds a high cost for devices requiring FDA clearance. Clinical validation studies, quality management system implementation, and regulatory submission preparation may add $50,000–$150,000+, depending on classification.
- Integration complexity varies based on existing infrastructure. Organizations with modern EHR systems and API-friendly architectures face lower integration costs than those requiring custom interfaces to legacy systems.
- Ongoing operational costs include cloud infrastructure, model monitoring, periodic retraining, and clinical quality assurance. Budget 15–25% of the initial development cost annually for maintenance and improvement.
Organizations seeking to manage costs effectively can hire AI developers through dedicated team models that provide specialized expertise without full-time hiring overhead. This approach proves particularly effective for organizations building initial capabilities before scaling internal teams.
With realistic budget expectations established, the next section covers best practices for successful implementation.
Best Practices for Implementing Computer Vision in Your Telehealth Platform
Successful computer vision implementations follow patterns that reduce risk and accelerate time-to-value. These practices emerge from lessons learned across healthcare AI projects.
1. Start with a focused use case
Begin with a single high-impact clinical scenario rather than attempting broad deployment across multiple applications simultaneously. Validate data availability, define clear success metrics tied to clinical outcomes, and build organizational capability before expanding scope.
2. Partner with clinical experts early
Engage clinicians throughout development to shape appropriate use cases, interface design, and workflow integration. Conduct prospective validation studies measuring actual clinical impact rather than relying solely on retrospective accuracy metrics.
3. Design for workflow integration
Build AI assistance that fits naturally into existing diagnostic workflows without requiring process changes. Implement progressive disclosure showing detail on demand and feedback mechanisms for clinicians to flag errors.
4. Plan for continuous improvement
Establish MLOps pipelines from the outset that monitor model performance in production, detect degradation, and support efficient retraining with proper version control and rollback capabilities.
Looking ahead, several emerging technologies will expand computer vision capabilities in telehealth.
Build Production-Ready Computer Vision for Your Telehealth Platform
From focused MVP to enterprise-scale deployment, our team delivers computer vision solutions that integrate seamlessly with clinical workflows.
The Future of Computer Vision in Telehealth
Computer vision in telemedicine continues advancing rapidly, with emerging technologies expanding diagnostic capabilities and improving accessibility. Several trends will shape the field over the coming years.
1. Multimodal AI integration
Multimodal AI combines visual analysis with other data types for comprehensive patient assessment. Systems that correlate medical images with clinical notes, lab results, vital signs, and genomic data provide richer diagnostic insights than any single modality alone. This convergence enables truly holistic remote patient evaluation where visual findings are interpreted within a complete clinical context.
2. Edge AI for mobile diagnostics
Edge AI pushes computer vision processing onto smartphones and portable devices. On-device inference eliminates connectivity requirements and latency concerns while enhancing privacy by keeping sensitive images local. Patients in resource-limited settings gain access to sophisticated visual diagnostics through devices they already own, democratizing specialist-level screening globally.
3. Federated learning for privacy-preserving improvement
Federated learning enables model improvement across institutions without centralizing sensitive medical images. Hospitals contribute to collective learning while maintaining local data control. This approach addresses both privacy concerns and the data scarcity that limits model development for rare conditions, enabling collaborative advancement without compromising patient confidentiality.
4. 3D reconstruction from standard video
3D reconstruction technology will enable volumetric assessment from consumer cameras. Wound depth measurement, facial symmetry analysis, and body composition assessment become possible without specialized imaging equipment. The technology dramatically expands what remote visual examination can evaluate, bringing capabilities previously requiring expensive hardware to standard telehealth encounters.
5. AR/VR integration for immersive examination
Augmented and virtual reality will transform remote physical examination. AR overlays guide patients through self-examination procedures while clinicians observe and direct. VR enables immersive telemedicine encounters where spatial understanding improves diagnostic capability, creating examination experiences that approach in-person quality despite physical distance.
These advances will make computer vision an increasingly essential component of telehealth platforms, enabling remote care that approaches in-person examination quality.
Partner with Space-O AI for Computer Vision in Telemedicine
Computer vision transforms telemedicine through automated image analysis, remote visual diagnostics, and clinical decision support capabilities. Healthcare organizations implementing these technologies expand specialist access, improve diagnostic accuracy, and deliver better patient outcomes while managing operational efficiency. The applications spanning dermatology, ophthalmology, radiology, and remote monitoring demonstrate proven clinical value.
Space-O AI brings 15+ years of experience building production-ready AI systems for healthcare and other regulated industries. With 500+ successful projects delivered, we understand both the technical complexity of computer vision development and the clinical validation requirements that determine real-world success. Our team has navigated FDA pathways and HIPAA compliance across multiple healthcare implementations.
Our team specializes in medical imaging AI, telehealth integration, and compliant healthcare deployments. We have built diagnostic support systems, achieving accuracy while integrating seamlessly with EHR systems and clinical workflows. Our expertise spans the full development lifecycle from data preparation through production monitoring and continuous improvement.
Ready to implement computer vision in your telemedicine platform? Schedule a free consultation to discuss your clinical use case, technical requirements, and implementation roadmap.
Frequently Asked Questions
1. What is computer vision in telemedicine, and how does it work?
Computer vision in telemedicine uses artificial intelligence algorithms to analyze medical images, video streams, and visual patient data during remote healthcare interactions. These systems enable clinicians to assess visual information that would traditionally require in-person examination.
Deep learning models process visual inputs to detect abnormalities, classify medical conditions, measure anatomical features, and monitor changes over time, providing real-time diagnostic and clinical decision support.
2. What are the main applications of computer vision in telehealth?
Computer vision supports a wide range of telehealth applications. Common use cases include dermatology image analysis for skin condition assessment, retinal imaging for diabetic eye screening, and radiology assistance for X-ray and CT scan interpretation.
Additional applications include physical therapy movement analysis, video-based vital sign monitoring, and digital pathology for remote tissue sample evaluation, addressing key limitations of traditional video-only telemedicine.
3. How accurate is AI-powered medical image analysis?
Accuracy varies based on the specific use case and quality of implementation. Well-validated computer vision systems achieve sensitivity and specificity rates of 90–95% for defined diagnostic tasks, often matching or exceeding specialist performance in controlled clinical studies.
Real-world performance depends on factors such as image quality, patient demographics, clinical workflows, and appropriate human oversight.
4. Is computer vision for telemedicine HIPAA compliant?
Computer vision solutions can be implemented in HIPAA-compliant environments, but compliance depends on secure system design rather than the technology alone. Key requirements include encrypted image storage and transmission, strict access controls, audit logging, and Business Associate Agreements with technology vendors.
Organizations must also ensure proper patient consent and ongoing compliance monitoring across the data pipeline.
5. How much does it cost to implement computer vision in a telehealth platform?
Implementation costs typically range from $75,000 to $300,000+, depending on system complexity and scope. Basic single-modality solutions usually cost between $75,000 and $120,000.
Advanced multi-modality platforms with regulatory clearance and deep clinical integration may exceed $300,000. Ongoing operational costs generally add 15–25% annually for maintenance, monitoring, and continuous improvement.
6. What are the regulatory requirements for medical computer vision systems?
Medical computer vision solutions are regulated as Software as a Medical Device (SaMD) by the FDA and international regulatory bodies. Requirements vary based on risk classification, intended clinical use, and condition severity.
Higher-risk applications require clinical validation and premarket regulatory review, while lower-risk tools may qualify for expedited approval pathways.
7. Can computer vision replace radiologists and other specialists?
No. Computer vision systems are designed to augment, not replace, clinical specialists. The technology excels at tasks such as screening, prioritization, measurement, and anomaly detection.
Clinicians remain responsible for contextual interpretation, complex clinical reasoning, and patient communication, ensuring safe and effective healthcare delivery.
Need Computer Vision for Telemedicine?
What to read next



