- 14 Ways Computer Vision Is Transforming Healthcare Today
- 1. Medical imaging analysis
- 2. Tumor detection and segmentation
- 3. Skin cancer detection
- 4. Diabetic retinopathy screening
- 5. Breast cancer screening
- 6. Lung disease detection
- 7. Surgical navigation and assistance
- 8. Patient monitoring and fall detection
- 9. Wound assessment and healing tracking
- 10. Pathology and microscopy analysis
- 11. Emergency room triage
- 12. Medication verification and dispensing
- 13. Vital signs monitoring
- 14. Medical research and clinical trials
- What Are the Key Benefits of Computer Vision in Healthcare?
- Implementing Computer Vision in Healthcare: Challenges and Solutions
- Transform Healthcare Operations with Space-O AI’s Computer Vision Expertise
- Frequently Asked Questions on Healthcare Computer Vision Applications
Computer Vision Applications in Healthcare: A Complete Guide for 2026

Have you ever wondered how AI can detect diseases faster than the human eye? Or how hospitals are using technology to monitor patients in real time and make surgeries more precise? The answer lies in computer vision, a cutting-edge technology that is transforming healthcare as we know it.
According to GrandViewResearch, the computer vision in healthcare market is expected to reach USD 15,600.8 million by 2030, reflecting the growing adoption of AI-powered imaging, diagnostics, and patient monitoring solutions. From analyzing medical scans to enabling real-time patient tracking, computer vision is helping healthcare providers deliver faster, more accurate, and safer care.
This blog dives into 14 key applications of computer vision in healthcare. As a leading computer vision development company, we have also covered our insights into the benefits and potential implementation challenges for seamless adoption. Let’s get started.
14 Ways Computer Vision Is Transforming Healthcare Today
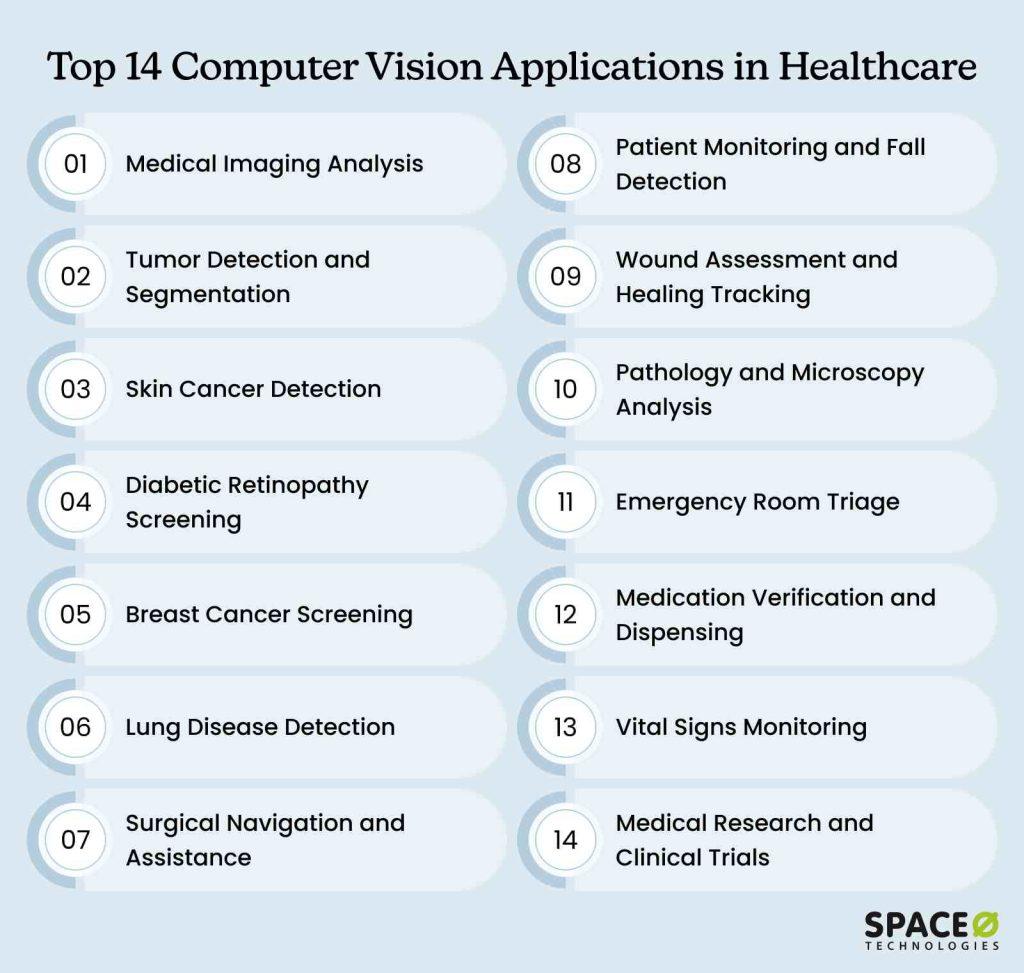
These applications of computer vision span five major categories: diagnostic imaging, patient monitoring, surgical assistance, hospital operations, and medical research. Each solves specific healthcare challenges while improving efficiency and outcomes.
Let’s explore the 14 most impactful computer vision application examples transforming healthcare today.
1. Medical imaging analysis
Challenge statement
Radiologists must review thousands of scans each week, often under intense time pressure. The repetitive nature of image interpretation leads to fatigue and declining focus, increasing the risk of missed abnormalities and diagnostic delays. As workloads grow, maintaining accuracy becomes harder, contributing to rising burnout across radiology departments.
How computer vision solves this
- AI acts as a tireless first reader, analyzing every image for abnormalities
- Flags concerning cases for immediate human review
- Highlights exactly where problems might exist
Key benefits
- Reduces diagnostic time
- Maintains or improves accuracy compared to human-only analysis
- Let’s radiologists focus on expertise where it matters most
- Never gets tired or distracted, even on the thousandth scan
| Real Impact: Patients get answers faster, doctors avoid burnout, and hospitals serve more people without compromising quality. |
2. Tumor detection and segmentation
Challenge statement
Oncologists need precise tumor boundaries to plan radiation therapy and surgical interventions, and manual segmentation is time-consuming, subject to inter-observer variability, and requires expert knowledge. Even millimeter-level errors in tumor mapping can result in healthy tissue damage or incomplete cancer treatment, directly affecting patient survival rates and quality of life.
How computer vision solves this
- Creates detailed 3D maps by analyzing medical scans
- Draws exact boundaries guiding treatment decisions
- Distinguishes malignant from benign by analyzing textures, shapes, and densities
Key benefits
- Ensures radiation beams precisely hit cancer cells while sparing healthy tissue
- Tracks tumor changes over time automatically
- Provides objective measurements for treatment adjustment
- Achieves millimeter-level precision critical for therapy planning
| Real Impact: Even small measurement errors can mean the difference between effective treatment and serious complications. |
Build Your Healthcare Computer Vision Solution With Experts
Work with Space-O AI’s experienced team to develop healthcare AI solutions that save time, reduce errors, and deliver results you can trust3. Skin cancer detection
Challenge statement
Dermatologists must identify dangerous melanomas among many benign lesions, a task that demands years of expertise and sharp visual judgment. Limited access to specialists, especially in rural areas, often delays diagnosis. Moreover, as early melanomas show few clear signs, even skilled clinicians can miss cancers or order unnecessary biopsies.
How computer vision solves this
- Analyzes smartphone photos of suspicious spots instantly
- Examines color, borders, asymmetry, and size using ABCDE criteria
- Trained on millions of skin photos representing diverse cases
Key benefits
- Serves as an early warning system for patients
- Provides consistent analysis regardless of clinic workload
- Enables screening in underserved areas without dermatologists
- Achieves accuracy comparable to board-certified specialists
| Real Impact: Catches warning signs early when treatment is most effective, potentially saving lives through early detection. |
4. Diabetic retinopathy screening
Challenge statement
Diabetes gradually damages retinal blood vessels without noticeable symptoms until vision loss becomes permanent. Regular screening can prevent blindness, but a shortage of ophthalmologists and time-intensive manual exams leaves many patients unscreened, blocking access to simple, sight-saving care.
How computer vision solves this
- Examines retinal photos for blood vessel damage
- Detects changes months or years before symptoms appear
- Grades disease severity for treatment prioritization
Key benefits
- Screening takes minutes instead of hours
- FDA-approved systems operate autonomously
- Integrates into routine diabetes checkups
- Works in rural areas lacking eye specialists
| Real Impact: Prevents blindness in diabetics through early detection when simple treatments still work. |
5. Breast cancer screening
Challenge statement
Mammography screening demands that radiologists review hundreds of images each day with sustained focus to catch subtle abnormalities. As fatigue sets in, accuracy declines, leading to missed cancers or unnecessary biopsies. Heavy workloads and limited capacity often create long wait times for results, delaying critical treatment.
How computer vision solves this
- Serves as a vigilant second pair of eyes on every mammogram
- Analyzes images for masses, calcifications, tissue changes
- Highlights suspicious areas deserving closer attention
Key benefits
- Reduces missed cancers during long screening sessions
- Detects cancers up to a year earlier in clinical trials
- Decreases false positives leading to unnecessary biopsies
- Enables smart triage, determining which cases need double-reading
| Real Impact: Earlier detection means less aggressive treatment and better survival rates. |
6. Lung disease detection
Challenge statement
Chest X-rays and CT scans reveal complex patterns linked to pneumonia, tuberculosis, lung cancer, and COVID-19. Radiologists must distinguish between these conditions that often appear similar, all while handling heavy case volumes.
Tiny nodules signaling early-stage lung cancer can easily blend into surrounding tissue, making accurate detection extremely challenging even for experienced specialists.
How computer vision solves this
- Reads visual stories in X-rays and CT scans
- Identifies infection, inflammation, and cancer patterns
- Quantifies lung damage extent
Key benefits
- Helped hospitals triage COVID-19 patients during the pandemic
- Finds tiny nodules easy to overlook
- Measures damage objectively and tracks recovery
- Provides data for treatment decisions
| Real Impact: Early detection of lung diseases significantly improves treatment outcomes and survival rates. |
7. Surgical navigation and assistance
Challenge statement
Surgeons operate in intricate 3D environments where vital nerves and vessels remain hidden beneath tissue. Achieving millimeter-level precision is critical, yet traditional surgery depends on interpreting 2D images and mental visualization. Limited visibility, anatomical variation, and natural hand tremor increase the risk of nerve damage, excessive bleeding, or procedural failure.
How computer vision solves this
- Provides augmented reality overlays showing anatomy beneath the surface
- Guides instrument placement with real-time visual feedback
- Tracks surgical tools and alerts if approaching critical structures
Key benefits
- Increases surgical precision and confidence
- Reduces complications from inadvertent damage
- Shortens the learning curve for complex procedures
- Enables minimally invasive approaches previously too risky
| Real Impact: Safer surgeries with better outcomes and faster patient recovery. |
8. Patient monitoring and fall detection
Challenge statement
Falls are a leading cause of injury and hospitalization among elderly patients, especially during understaffed nighttime hours. Conventional monitoring depends on intrusive wearables that patients often remove, and manual rounds that disrupt rest. At the same time, without constant observation, staff may miss critical moments, delaying response and worsening injuries.
How computer vision solves this
- Analyzes video feeds to detect unusual movements or positions
- Recognizes fall patterns and alerts staff instantly
- Monitors patient activity without intrusive wearables
Key benefits
- Prevents injuries through faster response times
- Maintains patient dignity without constant physical checks
- Reduces litigation from preventable falls
- Enables a single staff member to monitor multiple rooms
| Real Impact: Fewer fall-related injuries mean shorter hospital stays, lower costs, and better patient outcomes. |
Transform Patient Care with Proven AI Expertise
Our team builds computer vision applications that improve diagnostics, enhance monitoring, and streamline hospital operations9. Wound assessment and healing tracking
Challenge statement
Chronic wounds affect millions of patients with diabetes, vascular disease, and mobility limitations. Different caregivers measure wounds inconsistently, creating documentation that obscures healing trends or deterioration.
This lack of objective tracking makes it difficult for clinicians to determine treatment effectiveness, often leading them to continue ineffective approaches while wounds worsen and infection risks increase significantly.
How computer vision solves this
- Captures wound images with standard smartphone cameras
- Measures size, depth, tissue type automatically
- Tracks healing progress over time with objective data
Key benefits
- Provides a consistent assessment regardless of the evaluator
- Detects healing problems early
- Enables remote wound monitoring for home care patients
- Documents treatment effectiveness objectively
| Real Impact: Better wound management reduces complications, amputations, and healthcare costs while improving patient quality of life. |
10. Pathology and microscopy analysis
Challenge statement
Pathologists examine thousands of cells under a microscope to detect and grade tumors that determine treatment decisions. The process demands hours of intense focus and absolute precision, but human fatigue and subjective judgment introduce variability. Shortages of skilled professionals further delay diagnoses, directly affecting patient outcomes.
How computer vision solves this
- Analyzes digital slides at the cellular level
- Identifies cancer cells, grades tumors, and detects patterns
- Counts cells and measures features automatically
Key benefits
- Processes samples faster than human examination alone
- Maintains consistency across thousands of cells
- Free pathologists for complex diagnostic decisions
- Enables second opinions without physical slide shipping
| Real Impact: Faster, more accurate diagnoses lead to quicker treatment decisions and better patient outcomes. |
11. Emergency room triage
Challenge statement
Overcrowded emergency departments demand split-second assessments that determine treatment priority. Nurses must evaluate dozens of patients per hour under intense pressure, often with limited information. Subtle signs of life-threatening conditions can be missed, while overtriaging mild cases strains already limited resources.
How computer vision solves this
- Analyzes patient appearance, movement, and vital signs visually
- Identifies signs of severe conditions requiring immediate attention
- Assists triage nurses in rapid initial assessment
Key benefits
- Speeds triage during high-volume periods
- Reduces human error from fatigue or distraction
- Provides objective severity scoring
- Helps identify patients hiding pain or distress
| Real Impact: More accurate triage means critical patients get treatment faster while system capacity is optimized. For more accurate results, hire experienced computer vision developers to build custom triage solutions that integrate seamlessly with existing emergency systems and deliver superior accuracy. |
12. Medication verification and dispensing
Challenge statement
Medication errors cause thousands of preventable deaths annually despite multiple safety checkpoints. Pills look remarkably similar across drugs, while hospital pharmacies process hundreds of orders daily under intense time pressure. This creates opportunities for wrong medication, dose, or patient errors.
Even a single mistake can prove fatal, yet manual verification relies on human vigilance that’s vulnerable to fatigue and distraction.
How computer vision solves this
- Verifies pill identification by color, shape, and imprint
- Confirms correct medication matches prescription
- Monitors automated dispensing for accuracy
Key benefits
- Catches errors before reaching patients
- Verifies medications across the entire supply chain
- Reduces pharmacist workload for routine verification
- Provides an audit trail for compliance
| Real Impact: Fewer medication errors mean safer patients and reduced liability for healthcare facilities. |
13. Vital signs monitoring
Challenge statement
Traditional vital sign monitoring requires contact-based devices that limit mobility and increase infection risks. And, often, equipment shortages or gaps between manual checks leave patients unobserved for long periods. This leads to caretakers missing early signs of deterioration, which sometimes makes the patient’s condition critical.
How computer vision solves this
- Measures heart rate from subtle skin color changes
- Detects breathing rate from chest movement
- Assesses patient stress from facial expressions
Key benefits
- Enables contactless monitoring, reducing infection risk
- Works with standard cameras without special equipment
- Monitors multiple patients simultaneously
- Detects deterioration before traditional measurements
| Real Impact: Earlier detection of patient deterioration enables life-saving interventions and reduces ICU transfers. |
14. Medical research and clinical trials
Challenge statement
Medical research requires analyzing thousands of images to identify patterns and validate new therapies. Manual analysis creates bottlenecks lasting months or years, delaying life-saving discoveries.
Human measurement variability introduces bias that compromises research validity, while small teams lack resources for the massive datasets needed. This creates a painful clash between publication timelines and the reality of thorough analysis.
How computer vision solves this
- Processes large image datasets quickly and consistently
- Identifies patterns across populations
- Measures treatment effects objectively
Key benefits
- Accelerates medical research timelines
- Reduces human bias in measurements
- Enables larger-scale studies previously impractical
- Discovers patterns humans might miss
| Real Impact: Faster research means new treatments reach patients sooner, advancing medical science and improving care. |
Having explored these 14 powerful applications, let’s examine the concrete benefits driving healthcare organizations to invest in computer vision technology. Partnering with specialized computer vision development companies can help healthcare providers implement these applications while ensuring compliance with medical regulations and data privacy standards.
Looking for an Experienced Computer Vision Development Partner?
With 15+ years of computer vision development experience, we offer tailored healthcare AI solutions. Let Space-O AI build custom computer vision solutions that give your hospital smarter tools and faster insightsWhat Are the Key Benefits of Computer Vision in Healthcare?
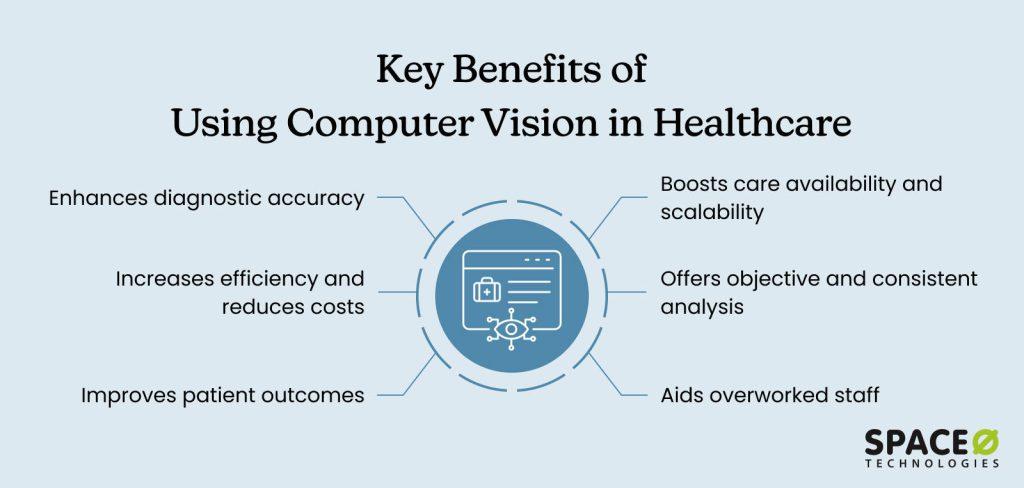
Healthcare organizations implementing computer vision realize substantial improvements across clinical and operational metrics. From reduced diagnostic errors and faster throughput to lower costs and better patient satisfaction, the technology delivers measurable ROI that justifies the initial investment. Let’s take a look at the top benefits:
1. Enhances diagnostic accuracy
Computer vision systems analyze medical images with consistency that humans can’t match. They detect subtle patterns indicating disease in early stages when treatment is most effective. Studies show AI-assisted diagnosis reduces errors and catches abnormalities that radiologists miss. This improved accuracy translates directly into better clinical outcomes and cost savings.
2. Increases efficiency and reduces costs
Beyond accuracy gains, automation handles routine analysis tasks, freeing medical professionals for complex cases requiring expertise. Hospitals process more patients without proportional staff increases. Faster diagnoses mean shorter hospital stays and reduced costs throughout the healthcare system. These efficiency improvements create capacity for treating more patients.
3. Improves patient outcomes
The combination of accuracy and efficiency drives measurable patient benefits. Earlier disease detection, more accurate diagnoses, and better surgical precision directly improve patient outcomes. Fewer complications mean faster recovery, better quality of life, and reduced mortality rates across various conditions. Patients experience care that’s both faster and more effective.
4. Boosts care availability and scalability
Unlike human staff, computer vision systems work continuously without fatigue, providing consistent analysis day and night. This technology scales easily to handle volume spikes without additional staffing costs. Rural facilities gain access to specialist-level analysis without geographic constraints. Round-the-clock availability ensures patients receive timely care regardless of when they arrive.
5. Offers objective and consistent analysis
Continuous operation also enables standardization across all cases. AI eliminates variability between different human evaluators. Every analysis follows the same criteria without influence from fatigue, stress, or subjective interpretation. This consistency improves quality and supports better clinical research. Healthcare organizations benefit from reproducible results they can trust.
6. Aids overworked staff
Finally, these systems address the human cost of healthcare delivery. Healthcare professionals face increasing workloads and burnout. Computer vision handles time-consuming screening and analysis tasks, allowing clinicians to focus on patient interaction and complex decision-making. This support improves job satisfaction and retention while ensuring clinicians work at the top of their expertise.
While the benefits are compelling, successful implementation requires addressing several important challenges head-on. Many healthcare organizations opt for computer vision consulting services to navigate these complexities with experts and avoid costly missteps. Let’s look at a few of these challenges.
Implementing Computer Vision in Healthcare: Challenges and Solutions
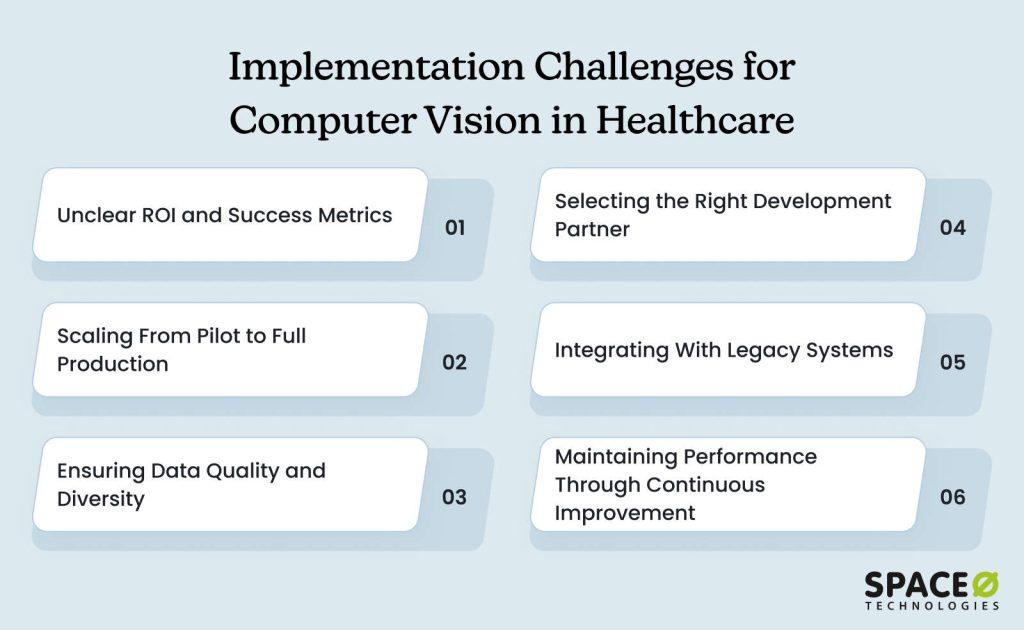
Strategic implementation requires addressing key challenges with proven solutions to ensure computer vision delivers expected benefits and ROI. From data quality and system integration to staff adoption and regulatory compliance, each challenge demands careful planning and execution to avoid common pitfalls.
1. Unclear ROI and success metrics
The problem
Organizations struggle to justify investment without measurable objectives or baseline data, making it impossible to demonstrate value or secure continued funding when stakeholders demand concrete evidence.
The solution
Identify specific problems computer vision solves with quantifiable impact and establish baseline measurements for accuracy, efficiency, and cost before implementation. Define concrete success metrics, including diagnostic accuracy improvements, time savings per case, cost reductions, and patient outcome enhancements to prove future value.
2. Scaling from pilot to full production
The problem
Pilot projects succeeding in controlled environments often fail at scale when unforeseen technical issues, workflow disruptions, and infrastructure limitations emerge during production deployment.
The solution
Start with a focused pilot in a controlled environment, testing across multiple departments and patient populations. Collect user feedback and refine based on real-world experience. During the pilot, evaluate server capacity, data storage requirements, processing speeds, and integration points to understand full-scale infrastructure needs.
Finally, build a deployment roadmap that phases expansion based on pilot learnings to identify potential issues before significant investment.
3. Ensuring data quality and diversity
The problem
AI systems require thousands of diverse, accurately labeled images representing actual patient populations. Many organizations lack sufficient data volume, face labeling inconsistencies, or have datasets skewed toward specific demographics, producing unreliable results during real-world deployment.
The solution
Invest significant time in data preparation with diverse, accurately labeled examples. Partner with clinical experts for accurate annotation while ensuring datasets represent your actual patient population across age, gender, ethnicity, and conditions. Audit existing data for quality and completeness, remembering your AI is only as good as the data it learns from.
4. Selecting the right development partner
The problem
Many technology vendors lack healthcare-specific expertise, leading to systems that fail regulatory requirements, don’t integrate with existing workflows, or miss critical clinical nuances that prevent successful implementation.
The solution
Select an AI development company like Space-O AI, with proven computer vision development expertise in the healthcare domain. Review detailed case studies from similar healthcare projects while verifying HIPAA compliance experience and FDA regulatory pathway understanding. Evaluate their team’s clinical domain knowledge to ensure they understand both technology and healthcare delivery realities.
5. Integrating with legacy systems
The problem
Healthcare organizations operate complex IT ecosystems with legacy EHR platforms, PACS systems, and clinical workflows that weren’t designed for AI integration, requiring seamless connections without disrupting existing operations or demanding complete infrastructure overhauls.
The solution
Work with IT teams from the project beginning, ensuring compatibility with existing systems. Map data flows, API integrations, and user interfaces carefully while planning for middleware where direct connections aren’t feasible. Involve medical professionals throughout development and test integrations thoroughly in staging environments to prevent costly rework.
6. Maintaining performance through continuous improvement
The problem
AI models degrade over time as clinical practices evolve, new equipment is introduced, imaging protocols change, or patient populations shift. Static systems become outdated, producing unreliable results that erode clinical trust while requiring ongoing resources and expertise.
The solution
Implement feedback mechanisms where clinicians flag incorrect predictions or edge cases. Establish regular performance monitoring to track accuracy, processing time, and user satisfaction. Use collected feedback for continuous model improvement while scheduling regular retraining with new data.
Not Sure How to Start with AI in Healthcare?
Partner with Space-O AI to ideate, develop, and implement reliable, high-performing healthcare computer vision solutions that deliver measurable resultsTransform Healthcare Operations with Space-O AI’s Computer Vision Expertise
Computer vision is transforming healthcare by making diagnostics faster and more precise, improving patient monitoring, supporting surgical procedures, and streamlining hospital operations. AI-powered imaging, real-time analysis, and predictive insights are helping healthcare providers deliver better outcomes while reducing costs and operational inefficiencies.
At Space-O AI, we specialize in end-to-end computer vision development for healthcare. Our capabilities include:
- Custom AI Model Development: Tailored computer vision algorithms for medical imaging, disease detection, and patient monitoring
- Data Annotation & Processing: High-quality medical data preparation for training accurate and reliable AI models
- Integration with Healthcare Systems: Seamless deployment with hospital IT infrastructure, EHR systems, and medical devices
- AR/VR & Robotics Assistance: AI-powered solutions that enhance precision in surgeries and rehabilitation
- Scalable & Compliant Solutions: Systems designed for regulatory compliance, security, and enterprise-level performance
- Continuous Support & Optimization: Ongoing monitoring, updates, and model improvements to ensure sustained accuracy and efficiency
With 15+ years of AI experience and 500+ successful projects, Space-O AI is your trusted partner for building innovative, reliable, and impactful computer vision solutions in healthcare.
Ready to transform your healthcare operations with AI? Connect with our experts today for a consultation and explore tailored computer vision solutions that meet your unique needs.
Frequently Asked Questions on Healthcare Computer Vision Applications
How accurate is computer vision in medical diagnosis?
Computer vision systems typically achieve 90-95% accuracy in many diagnostic tasks, often matching or exceeding human expert performance. Accuracy depends on the specific application, training data quality, and model architecture. FDA-approved systems for diabetic retinopathy detection demonstrate accuracy comparable to specialist ophthalmologists in clinical trials.
What is the cost of implementing computer vision in healthcare?
Implementation costs vary significantly by scope. Pilot projects typically cost $50,000–$150,000, while comprehensive hospital-wide systems can exceed $1 million. Costs include software development, hardware infrastructure, data preparation, integration, and training. Most organizations see positive ROI within 2-3 years.
Is computer vision replacing doctors and radiologists?
No. Computer vision augments medical professionals rather than replacing them. The technology handles routine screening and analysis, allowing doctors to focus on complex cases requiring human judgment and empathy. Final diagnostic decisions remain with qualified medical professionals.
How long does it take to implement computer vision solutions?
Implementation timelines range from 3-12 months, depending on project scope and organizational readiness. Focused pilot projects might launch in 3-6 months. Enterprise-wide deployments typically require 9-12 months, depending on data availability, integration complexity, and regulatory requirements.
How does computer vision ensure patient privacy and data security?
Healthcare computer vision systems implement multiple security layers, including end-to-end encryption, strict access controls, and HIPAA-compliant infrastructure. Many solutions use on-device processing to avoid sending sensitive data to cloud servers. Anonymization techniques remove identifying information from training data.
Let’s Bring Your Healthcare AI Idea to Life
What to read next



